Histiocitosis, una visión práctica para el dermatólogo
DOI:
https://doi.org/10.29176/2590843X.294Palabras clave:
histiocitos, histiocitosis de células de Langerhans, histiocitosis de células no LangerhansResumen
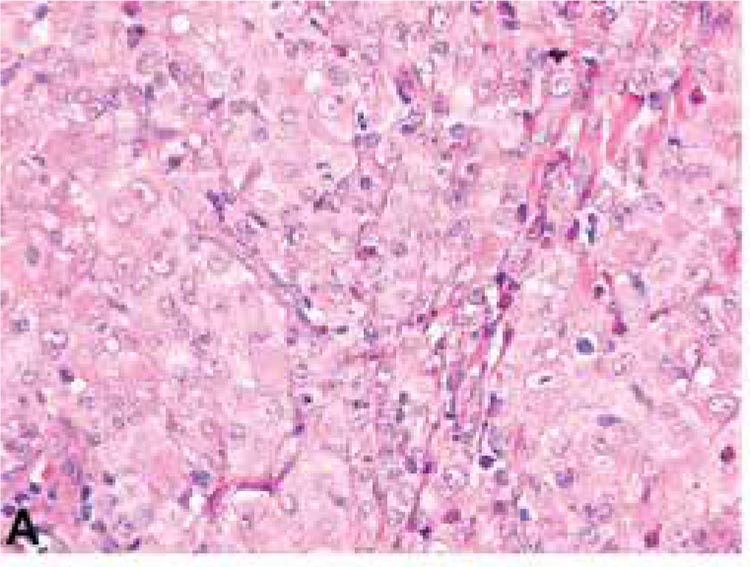
Las histiocitosis comprenden un grupo amplio de alteraciones caracterizadas por proliferación clonal anormal de histiocitos en los diferentes tejidos. Las manifestaciones clínicas pueden estar limitadas a la piel, incluso, pueden ser el primer signo de la enfermedad o pueden acompañarse de compromiso sistémico, como ocurre en la mayoría de los casos. La clasificación ha sido compleja y controversial a lo largo de la historia. La forma más sencilla de abordarlas las divide en histiocitosis de células de Langerhans y no Langerhans e histocitosis malignas. Se presenta una revisión de tema de las histiocitosis benignas desde un enfoque inmunohistoquímico útil y con los aspectos clínicos más relevantes para la práctica dermatológica.
Biografía del autor/a
Lina Vanessa Gómez
Médica, residente de III año de Dermatología, Universidad Pontificia Bolivariana, Medellín, Colombia.
Rodrigo Restrepo
Médico dermatopatólogo; jefe, Programa de Especialización en Dermatopatología, Universidad CES, Medellín, Colombia; profesor de Dermatopatología, Universidad Pontificia Bolivariana, Medellín, Colombia.
Natalia Buchely
Médica patóloga, Universidad Militar, fellow en Dermatopatología, Universidad CES, Medellín, Colombia.
Referencias bibliográficas
2. Shahlaee AH, Arceci RJ. Histiocytic disorders. En: Arceci R, Hann IM, Smith OP. Pediatric hematology. 3ed. Malden, Mass.: Blackwell Pub.; 2006.p.340-359
3. Goodman WT, Barret TL. Histiocytoses. En:Bolognia J, Lorizzo JL, Schaffer JV. Dermatology: [ExpertConsult]. 3rd ed. Edinburgh: Elsevier, Saunders; 2012.p.1529-1546.
4. Windebank K, Visser J, Nanduri V. Advances in the management of histiocytic disorders 2011. Paediatrics and Child Health. 2012;22:108-14.
5. Histiocytosis syndromes in children. Writing Group of the Histiocyte Society. Lancet Lond Engl. 1987;1:208-9.
6. Favara BE, Feller AC, Pauli M, Jaffe ES, Weiss LM, Arico M, et al. Contemporary classification of histiocytic disorders. The WHO Committee On Histiocytic/Reticulum Cell Proliferations. Reclassification Working Group of the Histiocyte Society. Med Pediatr Oncol. 1997;29:157-66.
7. El Demellawy D, Young JL, de Nanassy J, Chernetsova E, Nasr A. Langerhans cell histiocytosis: a comprehensive review. Pathology. 2015;47:294-301.
8. Goodlad J, Calonje E. Cutaneous lymphoproliferative diseases and related disorders. En: Calonje E, Brenn T, Lazzar A. MacKee PH, editores. McKee’s pathology of the skin: with clinical correlations. 4th ed. Edinburgh: Elsevier, Saunders; 2012.p.1311-1420
9. Nicholson HS, Egeler RM, Nesbit ME. The epidemiology of Langerhans cell histiocytosis. Hematol Oncol Clin North Am. 1998;12:379-84.
10. Kwon SH, Choi JW, Kim HJ, Youn SW. Langerhans cell histiocytosis: a retrospective analysis in a Korean tertiary hospital from 2003 to 2012. J Dermatol. 2013;40:824-8.
11. Guyot-Goubin A, Donadieu J, Barkaoui M, Bellec S, Thomas C, Clavel J. Descriptive epidemiology of childhood Langerhans cell histiocytosis in France, 2000-2004. Pediatr Blood Cancer. 2008;51:71-5.
12. Aricò M, Nichols K, Whitlock JA, Arceci R, Haupt R, Mittler U, et al. Familial clustering of Langerhans cell histiocytosis. Br J Haematol. 1999;107:883-8.
13. Edelbroek JR, Vermeer MH, Jansen PM, Stoof TJ, van der Linden MMD, Horváth B, et al. Langerhans cell histiocytosis first presenting in the skin in adults: frequent association with a second haematological malignancy. Br J Dermatol. 2012;167:1287-94.
14. Egeler RM, Neglia JP, Aricò M, Favara BE, Heitger A, Nesbit ME, et al. The relation of Langerhans cell histiocytosis to acute leukemia, lymphomas, and other solid tumors. The LCH-Malignancy Study Group of the Histiocyte Society. Hematol Oncol Clin North Am. 1998;12:369-78.
15. Ariza SA, Cardona AF, Rueda X. Histiocitiosis de células de Langerhans. Diez años de experiencia en el Instituto Nacional de Cancerología. Rev Asoc Colomb Dermatol. 2008;16:178-84.
16. Abla O, Egeler RM, Weitzman S. Langerhans cell histiocytosis: Current concepts and treatments. Cancer Treat Rev. 2010;36:354-9.
17. McClain K, Jin H, Gresik V, Favara B. Langerhans cell histiocytosis: lack of a viral etiology. Am J Hematol. 1994;47:16-20.
18. Toro AM, Rodrigo R, Ochoa A. Histiocitosis de células de Langerhans. Rev Asoc Colomb Dermatol. 2009;17:34-44.
19. Vaiselbuh SR, Bryceson YT, Allen CE, Whitlock JA, Abla O. Updates on histiocytic disorders. Pediatr Blood Cancer. 2014;61:1329-35.
20. Badalian-Very G, Vergilio J-A, Degar BA, MacConaill LE, Brandner B, Calicchio ML, et al. Recurrent BRAF mutations in Langerhans cell histiocytosis. Blood. 2010;116:1919-23.
21. Oishi N, Kondo T, Mochizuki K, Inoue T, Kasai K, Nakazawa T, et al. Localized Langerhans cell histiocytosis of the thymus with BRAF V600E mutation: a case report with immunohistochemical and genetic analyses. Hum Pathol. 2014;45:1302-5.
22. Paller A, Mancini AJ. Histiocytoses and Malignant Skin Diseases. En: Paller A, Mancini AJ. Hurwitz clinical pediatric dermatology. 4th ed. Edinburgh ; New York: Elsevier Saunders; 2011.p.219.233.
23. Munn S, Chu AC. Langerhans cell histiocytosis of the skin. Hematol Oncol Clin North Am. 1998;12:269-86.
24. Valdivielso M, Bueno C. [Langerhans cell histiocytosis]. Actas Dermo-Sifiliográficas. 2005;96:275-84.
25. Aruna DR, Pushpalatha G, Galgali S, Prashanthy null. Langerhans cell histiocytosis. J Indian Soc Periodontol. 2011;15:276-9.
26. Querings K, Starz H, Balda B-R. Clinical spectrum of cutaneous Langerhans’ cell histiocytosis mimicking various diseases. Acta Derm Venereol. 2006;86:39-43.
27. Mataix J, Betlloch I, Lucas-Costa A, Pérez-Crespo M, Moscardó-Guilleme C. Nail changes in Langerhans cell histiocytosis: a possible marker of multisystem disease. Pediatr Dermatol. 2008;25:247-51.
28. Haupt R, Minkov M, Astigarraga I, Schäfer E, Nanduri V, Jubran R, et al. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013;60:175-84.
29. Broadbent V, Gadner H, Komp DM, Ladisch S. Histiocytosis syndromes in children: II. Approach to the clinical and laboratory evaluation of children with Langerhans cell histiocytosis. Clinical Writing Group of the Histiocyte Society. Med Pediatr Oncol. 1989;17:492-5.
30. Valladeau J, Ravel O, Dezutter-Dambuyant C, Moore K, Kleijmeer M, Liu Y, et al. Langerin, a novel C-type lectin specific to Langerhans cells, is an endocytic receptor that induces the formation of Birbeck granules. Immunity. 2000;12:71-81.
31. Stierman SC, Spicknall KE. Dermatology diagnosis. Langerhans cell histiocytosis. Cutis. 2013;91:64, 67-9.
32. Hoeger PH, Nanduri VR, Harper JI, Atherton DA, Pritchard J. Long term follow up of topical mustine treatment for cutaneous langerhans cell histiocytosis. Arch Dis Child. 2000;82:483-7.
33. Sakai H, Ibe M, Takahashi H, Matsuo S, Okamoto K, Makino I, et al. Satisfactory remission achieved by PUVA therapy in Langerhans cell hisiocytosis in an elderly patient. J Dermatol. 1996;23:42-6.
34. Imafuku S, Shibata S, Tashiro A, Furue M. Cutaneous Langerhans cell histiocytosis in an elderly man successfully treated with narrowband ultraviolet B. Br J Dermatol. 2007;157:1277-9.
35. McClain KL, Kozinetz CA. A phase II trial using thalidomide for Langerhans cell histiocytosis. Pediatr Blood Cancer. 2007;48:44-9.
36. Tsambaos D, Georgiou S, Kapranos N, Monastirli A, Stratigos A, Berger H. Langerhans’ cell histiocytosis: complete remission after oral isotretinoin therapy. Acta Derm Venereol. 1995;75:62-4.
37. Steen AE, Steen KH, Bauer R, Bieber T. Successful treatment of cutaneous Langerhans cell histiocytosis with low-dose methotrexate. Br J Dermatol. 2001;145:137-40.
38. Girschikofsky M, Arico M, Castillo D, Chu A, Doberauer C, Fichter J, et al. Management of adult patients with Langerhans cell histiocytosis: recommendations from an expert panel on behalf of Euro-Histio-Net. Orphanet J Rare Dis. 2013;8:72.
39. Charles J, Beani J-C, Fiandrino G, Busser B. Major response to vemurafenib in patient with severe cutaneous Langerhans cell histiocytosis harboring BRAF V600E mutation. J Am Acad Dermatol. 2014;71:e97-9.
40. Gadner H, Minkov M, Grois N, Pötschger U, Thiem E, Aricò M, et al. Therapy prolongation improves outcome in multisystem Langerhans cell histiocytosis. Blood. 2013;121:5006-14.
41. Murcia J, Bárcenas W. Histiocitosis. Precop SCP. 2012. 11:36-48.
42. Weitzman S, Jaffe R. Uncommon histiocytic disorders: the non-Langerhans cell histiocytoses. Pediatr Blood Cancer. 2005;45:256-64.
43. Gelmetii C. Non-Langerhans Cell Histiocytosis. En: Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffel DJ, Wolff K. Fitzpatrick’s Dermatology in General Medicine. 8va ed. New York: McGraw-Hill Medical; 2012.p.1425-50
44. Chu AC. The confusing state of the histiocytoses. Br J Dermatol. 2000;143:475-6.
45. Rodriguez-Jurado R, Duran-McKinster C, Ruiz-Maldonado R. Benign cephalic histiocytosis progressing into juvenile xanthogranuloma: a non-Langerhans cell histiocytosis transforming under the influence of a virus? Am J Dermatopathol. 2000;22:70-4.
46. Zelger BW, Sidoroff A, Orchard G, Cerio R. Non-Langerhans cell histiocytoses. A new unifying concept. Am J Dermatopathol. 1996;18:490-504.
47. Newman B, Hu W, Nigro K, Gilliam AC. Aggressive histiocytic disorders that can involve the skin. J Am Acad Dermatol. 2007;56:302-16.
48. Lovato L, Salerni G, Puig S, Carrera C, Palou J, Malvehy J. Adult xanthogranuloma mimicking basal cell carcinoma: dermoscopy, reflectance confocal microscopy and pathological correlation. Dermatol Basel Switz. 2010;220:66-70.
49. Szczerkowska-Dobosz A, Kozicka D, Purzycka-Bohdan D, Biernat W, Stawczyk M, Nowicki R. Juvenile xanthogranuloma: a rare benign histiocytic disorder. Postȩpy Dermatol Alergol. 2014;31:197-200.
50. Gianotti F, Caputo R. Histiocytic syndromes: a review. J Am Acad Dermatol. 1985;13:383-404.
51. Gianotti F. Cutaneous proliferative histiocytosis in children. G Ital Dermatol Venereol. 1980;115:101-5.
52. Samara WA, Khoo CT, Say EA, Saktanasate J, Eagle RC Jr, Shields JA, et al. Juvenile Xanthogranuloma Involving the Eye and Ocular Adnexa: Tumor Control, Visual Outcomes, and Globe Salvage in 30 Patients. Ophthalmology. 2015;122:2130-8
53. Murphy JT, Soeken T, Megison S, Perez E. Juvenile xanthogranuloma: diverse presentations of noncutaneous disease. J Pediatr Hematol Oncol. 2014;36:641-5.
54. Fenot M, Stalder J-F, Barbarot S. Juvenile xanthogranulomas are highly prevalent but transient in young children with neurofibromatosis type 1. J Am Acad Dermatol. 2014;71:389-90.
55. Jans SRR, Schomerus E, Bygum A. Neurofibromatosis type 1 diagnosed in a child based on multiple juvenile xanthogranulomas and juvenile myelomonocytic leukemia. Pediatr Dermatol. 2015;32:e29-32.
56. Alan Arbuckle H, Prok L. Case report--papular xanthoma in a 10-year-old female with abnormal lipid profile. Pediatr Dermatol. 2010;27:86-8.
57. Breier F, Zelger B, Reiter H, Gschnait F, Zelger BWH. Papular xanthoma: a clinicopathological study of 10 cases. J Cutan Pathol. 2002;29:200-6.
58. Cardoso F, Serafini NB, Reis BD, Nuñez MDG, Nery JA da C, Lupi O. Generalized eruptive histiocytoma: a rare disease in an elderly patient. An Bras Dermatol. 2013;88:105-8.
59. Kazi N, Bernert R, Moussa C, Magro C. A case of generalized eruptive histiocytosis in a 23-year-old man. Dermatol Online J. 2014;20(8). pii: 13030/qt39v75449.
60. Vázquez-Blanco M, Peteiro C, Toribio J. [Generalized eruptive histiocytoma]. Actas Dermo-Sifiliográficas. 2006;97:35-8.
61. Koca R, Bektaş S, Altinyazar HC, Sezer T. Benign cephalic histiocytosis: a case report. Ann Dermatol. 2011;23:508-11.
62. Lange M, Iżycka-Świeszewska E, Michajłowski I, Barańska-Rybak W. Benign cephalic histiocytosis. Cutis. 2015;95:E15-7.
63. Samson JF, Libu GK, Philip M, Simi PS. Benign cephalic histiocytosis. Indian Dermatol Online J. 2013;4:300-1.
64. Weston WL, Travers SH, Mierau GW, Heasley D, Fitzpatrick J. Benign cephalic histiocytosis with diabetes insipidus. Pediatr Dermatol. 2000;17:296-8.
65. Saez-De-Ocariz M, Lopez-Corella E, Duran-McKinster C, Orozco-Covarrubias L, Ruiz-Maldonado R. Benign cephalic histiocytosis preceding the development of insulin-dependent diabetes mellitus. Pediatr Dermatol. 2006;23:101-2.
66. Nofal A, Assaf M, Tawfik A, Elsayed N, Nofal E, Elnakib N, et al. Progressive nodular histiocytosis: a case report and literature review. Int J Dermatol. 2011;50:1546-51.
67. Kunimoto K, Uede K, Furukawa F. Progressive nodular histiocytosis. J Dermatol. 2010;37:1071-3.
68. Hilker O, Kovneristy A, Varga R, Neubert T, Wesselmann U, Flaig MJ, et al. Progressive nodular histiocytosis. J Dtsch Dermatol Ges J Ger Soc Dermatol JDDG. 2013;11:301-7.
69. Caputo R, Marzano AV, Passoni E, Berti E. Unusual variants of non-Langerhans cell histiocytoses. J Am Acad Dermatol. 2007;57:1031-45.
70. Ansarin H, Berenji Ardestani H, Tabaie SM, Shayanfar N. Xanthoma disseminatum with tumor-like lesion on face. Case Rep Dermatol Med. 2014;2014:621798.
71. Attia AM, Bakry OA, Mohamed EE. Xanthoma disseminatum: a progressive case with multisystem involvement. J Postgrad Med. 2014;60:69-71.
72. Pinto ME, Escalaya GR, Escalaya ME, Pinto JL, Chian CA. Xanthoma disseminatum: case report and literature review. Endocr Pract Off J Am Coll Endocrinol Am Assoc Clin Endocrinol. 2010;16:1003-6.
73. Seastrom S, Bookout A, Hogan DJ. Necrobiotic xanthogranuloma without a monoclonal gammopathy. Cutis. 2014;94:293-6.
74. Pipkin CA, Lio PA. Cutaneous manifestations of internal malignancies: an overview. Dermatol Clin. 2008;26:1-15, vii.
75. Wood AJ, Wagner MVU, Abbott JJ, Gibson LE. Necrobiotic xanthogranuloma: a review of 17 cases with emphasis on clinical and pathologic correlation. Arch Dermatol. 2009;145:279-84.
76. Kim M-S, Kim C-H, Choi S-J, Won C-H, Chang S-E, Lee M-W, et al. Erdheim-chester disease. Ann Dermatol. 2010;22:439-43.
77. Volpicelli ER, Doyle L, Annes JP, Murray MF, Jacobsen E, Murphy GF, et al. Erdheim-Chester disease presenting with cutaneous involvement: a case report and literature review. J Cutan Pathol. 2011;38:280-5.
78. Chisolm SS, Schulman JM, Fox LP. Adult Xanthogranuloma, Reticulohistiocytosis, and Rosai-Dorfman Disease. Dermatol Clin. 2015;33:465-72
79. Islam AD, Naguwa SM, Cheema GS, Hunter JC, Gershwin ME. Multicentric reticulohistiocytosis: a rare yet challenging disease. Clin Rev Allergy Immunol. 2013;45:281-9.
80. Selmi C, Greenspan A, Huntley A, Gershwin ME. Multicentric reticulohistiocytosis: a critical review. Curr Rheumatol Rep. 2015;17:511.
81. Miceli A, Cleaver N, Spizuoco A. Rosai-Dorfman disease. Cutis. 2015;96:16, 39-40.
82. Kwinter J, DeKoven J. Generalized eruptive histiocytoma treated with isotretinoin. J Cutan Med Surg. 2009;13:146-50.
83. Lan Ma H, Metze D, Luger TA, Steinhoff M. Successful treatment of generalized eruptive histiocytoma with PUVA. J Dtsch Dermatol Ges J Ger Soc Dermatol JDDG. 2007;5:131-4.
84. Wood GS, Hu CH, Beckstead JH, Turner RR, Winkelmann RK. The indeterminate cell proliferative disorder: report of a case manifesting as an unusual cutaneous histiocytosis. J Dermatol Surg Oncol. 1985;11:1111-9.
85. Ratzinger G, Burgdorf WHC, Metze D, Zelger BG, Zelger B. Indeterminate cell histiocytosis: fact or fiction? J Cutan Pathol. 2005;32:552-60.
86. Rodríguez-Jurado R, Vidaurri-de la Cruz H, Durán-Mckinster C, Ruíz-Maldonado R. Indeterminate cell histiocytosis. Clinical and pathologic study in a pediatric patient. Arch Pathol Lab Med. 2003;127:748-51.
87. Tóth B, Katona M, Hársing J, Szepesi A, Kárpáti S. Indeterminate cell histiocytosis in a pediatric patient: successful treatment with thalidomide. Pathol Oncol Res POR. 2012;18:535-8.
88. Martín JM, Jordá E, Martín-Gorgojo A, Beteta G, Monteagudo C. Histiocytosis with mixed cell populations. J Cutan Pathol. 2016;43:456-60.
89. Calatayud M, Güell JL, Gris O, Puig J, Arrondo E, Huguet P. Ocular involvement in a case of systemic indeterminate cell histiocytosis: a case report. Cornea. 2001;20:769-71.
90. Ventura F, Pereira T, da Luz Duarte M, Marques H, Pardal F, Brito C. Indeterminate cell histiocytosis in association with acute myeloid leukemia. Dermatol Res Pract. 2010;2010:569345.
91. Vener C, Soligo D, Berti E, Gianelli U, Servida F, Ceretti E, et al. Indeterminate cell histiocytosis in association with later occurrence of acute myeloblastic leukaemia. Br J Dermatol. 2007;156:1357-61.
92. Haimovic A, Chernoff K, Hale CS, Meehan SA, Schaffer JV. Indeterminate cell histiocytosis that presented clinically as benign cephalic histiocytosis. Dermatol Online J. 2014;20(12). pii: 13030/qt23d5k96k.
93. Wang C-H, Chen G-S. Indeterminate cell histiocytosis: a case report. Kaohsiung J Med Sci. 2004;20:24-30.
94. Logemann N, Thomas B, Yetto T. Indeterminate cell histiocytosis successfully treated with narrowband UVB. Dermatol Online J. 2013;19:20031.
95. Fournier J, Ingraffea A, Pedvis-Leftick A. Successful treatment of indeterminate cell histiocytosis with low-dose methotrexate*. J Dermatol. 2011;38:937-9.
96. Burns MV, Ahmed A, Callahan GB, Le LQ, Cockerell C. Treatment of indeterminate cell histiocytosis with pravastatin. J Am Acad Dermatol. 2011;64:e85-86.
97. Malhomme de la Roche H, Lai-Cheong JE, Calonje E, Davies M, Morris S, Whittaker SJ. Indeterminate cell histiocytosis responding to total skin electron beam therapy. Br J Dermatol. 2008;158:838-40.
Cómo citar
Descargas