Perspective of dermatology and COVID-19
DOI:
https://doi.org/10.29176/2590843X.1487Keywords:
Coronavirus infections, Skin manifestations, Pandemics, Health personnel, Dermatology, TeledermatologyAbstract
The scientific evidence of cutaneous manifestation produced by the new SARS-CoV-2 coronavirus (COVID-19) is increasing. The exacerbation of pre-existing skin diseases and injuries due to prolonged use of personal protection elements are emerging. Dermatology specialists must know them and guide in prevention and treatment as well.
This article reviews the skin manifestations in patients with COVID-19, cutaneous lesions that have arisen in health workers, the perspective of teledermatology as a tool to fight against the pandemics, some special considerations, and protection of skin and mucous membranes.
Author Biographies
Natalia Calvache
Residente de Dermatología, Universidad Libre de Cali, Colombia. Grupo de Investigación en Dermatología (GRINDERM), Universidad Libre de Cali, Colombia.
Juan Carlos Jaimes
Residente de Dermatología, Universidad Libre de Cali, Colombia. Grupo de Investigación en Dermatología (GRINDERM), Universidad Libre de Cali, Colombia.
Paula Candelo
Residente de Dermatología, Universidad Libre de Cali, Colombia. Grupo de Investigación en Dermatología (GRINDERM), Universidad Libre de Cali, Colombia.
Christian Prada
Residente de Dermatología, Universidad Libre de Cali, Colombia. Grupo de Investigación en Dermatología (GRINDERM), Universidad Libre de Cali, Colombia.
Yurani Pineda
Residente de Dermatología, Universidad Libre de Cali, Colombia. Grupo de Investigación en Dermatología (GRINDERM), Universidad Libre de Cali, Colombia.
Erika Peña
Residente de Dermatología, Universidad Libre de Cali, Colombia. Grupo de Investigación en Dermatología (GRINDERM), Universidad Libre de Cali, Colombia.
Eduardo Fierro
Grupo de Investigación en Dermatología (GRINDERM), Universidad Libre de Cali, Colombia. Dermatólogo-oncólogo; Docente, Universidad Libre de Cali, Colombia.
References
2. Gorbalenya AE, Baker SC, Baric RS, de Groot RJ, Drosten C, Gulyaeva AA, Haagmans BL, Lauber C, Leontovich AM, Neuman BW, Penzar D, Perlman, et al. Severe acute respiratory syn drome related coronavirus: The species and its viruses a statement of the Coronavirus Study Group. bioRxiv. 2020.02.07.937862; doi: https://doi.org/10.1101/2020.02.07.937862.
3. Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, Liu L, Shan H, Lei C, Hui D, Du B, Li L, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708-20. doi: 10.1056/NEJMoa2002032.
4. Yao X, Li T, He Z, Ping Y, Liu H, Yu S, Mou HM, Wang LH, Zhang HR, Fu WJ, Luo T, Liu F, et al. [A pathological report of three COVID-19 cases by minimally invasive autopsies]. Zhonghua Bing Li Xue Za Zhi. 2020;49(5):411-7. doi: 10.3760/cma.j.cn112151-20200312-00193.
5. Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ, Akdis C, Gao YD. Clinical characteris¬tics of 140 patients infected with SARS-CoV-2 in Wuhan, China [Internet]. Allergy. 2020. doi: 10.1111/all.14238.
6. Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Vene¬reol. 2020;34(5):e212-3. doi: 10.1111/jdv.16387.
7. Hoenig L, Pereira F. Rash as a Clinical Ma¬nifestation of COVID 19 Photographs of a Patient. Clin Dermatol. 2020. doi:10.1016/j.clindermatol.2020.04.001.
8. Joob B, Wiwanitkit V. COVID-19 can pre¬sent with a rash and be mistaken for dengue. J Am Acad Dermatol. 2020;82(5):e177. doi: 10.1016/j.jaad.2020.03.036.
9. Marzano AV, Genovese G, Fabbrocini G, Pi¬gatto P, Monfrecola G, Piraccini BM, Veraldi S, Rubegni P, Cusini M, Caputo V, Rongioletti F, Berti E, et al. Varicella-like exanthem as a spe¬cific COVID-19-associated skin manifestation: multicenter case series of 22 patients. J Am Acad Dermatol. 2020;S0190-9622(20)30657-5. doi: 10.1016/j.jaad.2020.04.044.
10. Manalo IF, Smith MK, Cheeley J, Jacobs R. A Dermatologic Manifestation of COVID-19: Transient Livedo Reticularis. J Am Acad Der¬matol. 2020;S0190-9622(20)30558-2. doi: 10.1016/j.jaad.2020.04.018.
11. Zhang Y, Cao W, Xiao M, Li Y, Yang Y, Zhao J, Zhou X, Jiang W, Zhao YQ, Zhang SY, Li TS. [Clinical and coagulation characteristics of 7 patients with cri¬tical COVID-2019 pneumonia and acro-ischemia]. Zhonghua Xue Ye Xue Za Zhi. 2020;41(0):E006. doi: 10.3760/cma.j.issn.0253-2727.2020.0006.
12. Mazzotta F, Troccoli T. Acute acro-ischemia in the at the time of COVID-19. Eur J Pediat Der¬matol. 2020;(Monday´s case):3-5.
13. Shi Y, Yu X, Zhao H, Wang H, Zhao R, Sheng J. Host susceptibility to severe COVID-19 and establish¬ment of a host risk score: Findings of 487 cases outside Wuhan. Crit Care. 2020;24(1):108. doi: 10.1186/s13054-020-2833-7.
14. Wambier CG, Goren A. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection is likely to be androgen mediated. J Am Acad Dermatol. 2020;S0190-9622(20)30608-3. doi:10.1016/j.jaad.2020.04.032.
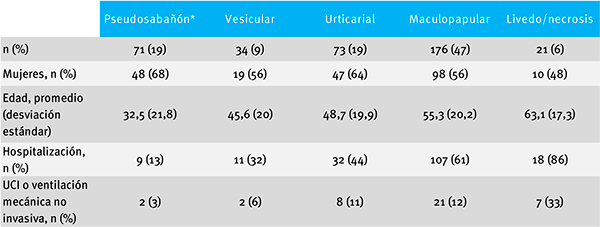
15. Galvan Casas C, Catala A, Carretero Hernandez G, Rodriguez-Jimenez P, Fernandez Nieto D, Ro¬driguez-Villa Lario A, Navarro Fernandez I, Ruiz-Villaverde R, Falkenhain D, Llamas Velasco M, García-Gavin J, Baniandrés O, et al. Classification of the cutaneous manifestations of COVID-19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol. 2020. doi: 10.1111/bjd.19163.
16. Zengarini C, Orioni G, Cascavilla A, Horna So¬lera C, Fulgaro C, Misciali C, Patrizi A, Gaspari V. Histological pattern in Covid-19 induced viral rash. J Eur Acad Dermatol Venereol. 2020. doi: 10.1111/jdv.16569.
17. Chawla S. COVID-19: Challenges and op¬portunities for dermatology response. J Dermatolog Treat. 2020;31(4):326. doi: 10.1080/09546634.2020.1751040.
18. Elston DM. Occupational skin disease among healthcare workers during the Co¬ronavirus (COVID-19) epidemic. J Am Acad Dermatol. 2020;82(5):1085-1086. doi: 10.1016/j.jaad.2020.03.012.
19. Darlenski R, Tsankov N. Covid-19 pan¬demic and the skin - What should derma¬tologists know? Clin Dermatol. 2020. doi: https://doi.org/10.1016/j.clindermatol.2020.03.012.
20. Lin P, Zhu S, Huang Y, Li L, Tao J, Lei T, Song J, Liu D, Chen L, Shi Y, Jiang S, Liu Q, et al. Ad¬verse Skin Reactions Among Healthcare Wor¬kers During the Coronavirus Disease 2019 Outbreak: A Survey in Wuhan and Its Su¬rrounding Regions. Br J Dermatol. 2020. doi: 10.1111/bjd.19089.
21. Lan J, Song Z, Miao X, Li H, Li Y, Dong L, Yang J, An X, Zhang Y, Yang L, Zhou N, Yang L, et al. Skin damage among healthcare wor¬kers managing coronavirus disease-2019. J Am Acad Dermatol. 2020;82(5):1215-6. doi: 10.1016/j.jaad.2020.03.014.
22. Villani A, Scalvenzi M, Fabbrocini G. Tele¬dermatology: a useful tool to fight COVID-19. J Dermatolog Treat. 2020;31(4):325. doi:10.1080/09546634.2020.1750557.
23. Chawla S. COVID-19: Challenges and op¬portunities for dermatology response. J Dermatolog Treat. 2020;31(4):326. doi:10.1080/09546634.2020.1751040.
24. Lee I, Kovarik C, Tejasvi T, Pizarro M, Lipoff JB. Telehealth: Helping Your Patients and Prac¬tice Survive and Thrive During the COVID-19 Crisis with Rapid Quality Implementation. J Am Acad Dermatol. 2020;82(5):1213-4. doi: 10.1016/j.jaad.2020.03.052.
25. Resolución 2654 de 2019. Por la cual se establecen disposiciones para la telesalud y parámetros para la práctica de la telemedicina en el país. Ministerio de Salud y Protección Social de Colombia.
26. Ministerio de Salud y Protección Social. Li¬neamientos para la detección y manejo de casos de COVID-19 por los prestadores de ser¬vicios de salud en Colombia. Ministerio de Salud y Protección social; 2020. Disponible en: https://bit.ly/2zg242J.
27. Jakhar D, Kaur I, Kaul S. Art of performing der¬moscopy during the times of coronavirus disease (COVID-19): simple change in approach can save the day! J Eur Acad Dermatol Venereol. 2020. doi: 10.1111/jdv.16412.
28. Yan Y, Chen H, Chen L, Cheng B, Diao P, Dong L, Gao X, Gu H, He L, Ji C, Jin H, Lai W, et al. Consensus of Chinese experts on protection of skin and mucous membrane barrier for health-care workers fighting against coronavirus di¬sease 2019. Dermatol Ther. 2020;e13310. doi:10.1111/dth.13310.
29. Cuevas-López L, Ayala J, Velásquez-Jiménez O, Navarro-Alean J, González-Higuera L, Zurita N, Hernández-Restrepo JD, Herrera Chaparro J, Ortiz D, Zuluaga-Zuluaga M, Bonilla-Ardila G. Recomendaciones para el manejo de los pa¬cientes quirúrgicos urgentes durante la pandemia COVID-19. Rev Colomb Cir. 2020;35:143-52. doi: 10.30944/20117582.619.
30. National Comprenhensive Cancer Net¬work NCCN. Advisory Statement for Non-Melanoma Skin Cancer Care During the COVID-19 Pandemic [Internet]. Disponible en: https://www.nccn.org/covid-19/.
31. Der Sarkissian SA, Kim L, Veness M, Yiasemides E, Sebaratnam DF. Recommendations on dermato¬logic surgery during the COVID-19 pandemic. J Am Acad Dermatol. 2020;S0190-9622(20)30610-1. doi: 10.1016/j.jaad.2020.04.034.
32. Skulsky S, O’Sullivan B, McArdle O, Leader M, Roche M, Conlon P, O´Neill JP. Review of high-risk features of cutaneous squamous cell carcinoma and dis¬crepancies between the American Joint Committee on Cancer and NCCN Clinical Practice Guidelines In Oncology. Head Neck. 2017;39(3):578-94. doi: 10.1002/hed.24580.
33. Villani A, Fabbrocini G, Costa C, Scalvenzi M. Patients with advanced basal cell carcinomas in treatment with sonic hedgehog inhibitors du¬ring the coronavirus disease 2019 (COVID-19) pe¬riod: Management and adherence to treatment. J Am Acad Dermatol. 2020;82(6):e205. doi: 10.1016/j.jaad.2020.03.057.
34. Zic J, Ai W, Akilov O, Carter J, Duvic M, Foss F, Girardi M, Gru AA, Kim E, Musiek A, Olsen EA, Schieke SM, et al. United States Cuta¬neous Lymphoma Consortium. Recommenda¬tions for Treatment of Cutaneous Lymphomas During the COVID-19 Pandemic. J Am Acad Dermatol. 2020;S0190-9622(20)30662-9. doi: 10.1016/j.jaad.2020.04.049.
35. Price K, Frew J, Hsiao J, Shi V. COVID-19 and immu¬nomodulator/ immunosuppressant use in dermato¬logy. J Am Acad Dermatol. 2020;82(5):e173-e175. doi: 10.1016/j.jaad.2020.03.046.
36. Lebwohl M, Rivera-Oyola R, Murrell DF. Should bio¬logics for psoriasis be interrupted in the era of COVID-19? J Am Acad Dermatol. 2020;82(5):1217-8. doi: 10.1016/j.jaad.2020.03.031.
37. Di Lernia V. Biologics for psoriasis du¬ring COVID-19 outbreak. J Am Acad Dermatol. 2020;82(6):e217-8. doi: 10.1016/j.jaad.2020.04.004.
38. World Health Organization. Infection pre¬vention and control during health care when COVID-19 is suspected: interim gui-dance, 19 March 2020. Disponible en: https://bit.ly/2A2Ao1a.
How to Cite
Downloads
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2020 Revista de la Asociación Colombiana de Dermatología y Cirugía Dermatológica

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |







