Lymphocutaneous syndrome of infectious cause: narrative review and diagnostic approach
DOI:
https://doi.org/10.29176/2590843X.1489Abstract
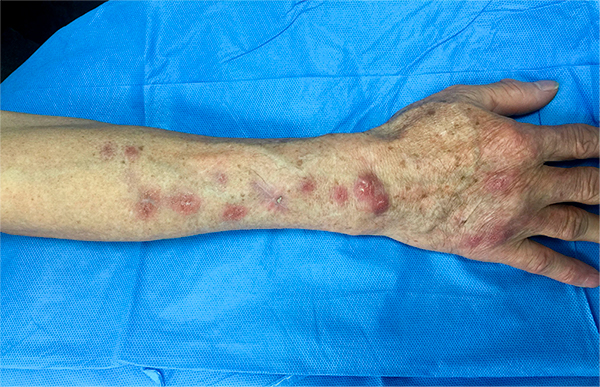
Introduction: Lymphocutaneous syndrome is a very characteristic clinical form of lymphangitis that presents with subcutaneous inflammatory nodules that follow a path. Multiple infectious pathologies that could have this clinical presentation have been described and their diagnostic approach is key to successful treatment.
Methods: A search was made in PubMed MEDLINE and later a narrative review describing the different infectious etiologies of the lymphocutaneous syndrome.
Results: Lymphocutaneous syndrome can have multiple causes, among which are fungal, bacterial, infections by typical or atypical mycobacteria, and parasites, being Sporothrix schenckii, Nocardia brasiliensis, Mycobacterium marinum and Leishmania sp. the most frequently associated agents. To determine its etiology, it is necessary to consider aspects in the anamnesis (origin, occupation, time of evolution, history of trauma), semiology of the lesions, associated symptoms and in many cases diagnostic confirmation with skin biopsies, culture or Gram stain, or other additional studies. Its treatment should be directed and generally due to the involvement of lymphatic pathways, it is extended for a longer time compared to localized infections.
Conclusions: when we are faced with a patient with findings suggestive of lymphocutaneous syndrome, we must consider multiple infectious etiologies. In order to make the diagnostic approach easier, we propose to classify the causal agents into 4 main groups: fungal, bacterial, mycobacterial, and parasitic infections.
Author Biographies
Claudia M. Arenas Soto
Dermatóloga, Especialista en docencia universitaria, Universidad Militar Nueva Granada.
Daniela Chaparro Reyes
Residente Dermatología, Pontificia Universidad Javeriana.
Angela M. Mariño Álvarez
Dermatóloga, Universidad Militar Nueva Granada.
Alejandra Sandoval
Residente Dermatología, Fundación Universitaria Sanitas.
References
2. Smego RA, Castiglia M, Asperilla MO. Lympho¬cutaneous Syndrome. A Review of Non-Sporo¬thix Causes. Medicine. 1999;78(1):38-63. doi: 10.1097/00005792-199901000-00004.
3. DiNubile MJ. Nodular lymphangitis: A dis¬tinctive clinical entity with finite etiologies. Curr Infect Dis Rep. 2008;10(5):404-10. doi: 10.1007/s11908-008-0065-0.
4. Tobin EH, William W. Sporotrichoid lymphocuta¬neous infections: Etiology, diagnosis and therapy. Am Fam Physician. 2001;63(2):326-32.
5. Tirado-Sánchez A, Bonifaz A. Nodu¬lar Lymphangitis (Sporotrichoid Lympho¬cutaneous Infections). Clues to Differen¬tial Diagnosis. J Fungi. 2018;4(2):56. doi: 10.3390/jof4020056.
6. Inamadar A, Palit A. Primary cutaneous nocardio¬sis : A case study and review. Indian J Dermatol Venereol Leprol. 2003;69(6):386-91.
7. Wilson J. Comparative immunologic aspects of deep fungus disease. Cutis. 1975;16:231-4.
8. Schwatrz J, Baum G. Primary cutaneous my¬coses. Arch Dermatol. 1955;71(2):143-9. doi: 10.1001/archderm.1955.01540260001001.
9. Gaviria-Giraldo CM, Cardona Castro N. Espo¬rotricosis y cromoblastomicosis: revisión de la literatura. Rev Univ CES. 2017;31(1):77-91. doi: http://dx.doi.org/10.21615/cesmedicina.31.1.8.
10. Queiroz-Telles F, Mcginnis MR, Salkin I, Graybill JR. Subcutaneous mycoses. In¬fect Dis Clin N Am. 2003;17(1):59-85. doi: 10.1016/s0891-5520(02)00066-1.
11. Carrasco-Zuber JE, Navarrete-Dechent C, Bonifaz A, Fich F, Vial-Letelier V, Berroeta-Mauriziano D. Cutaneous Involvement in the Deep Mycoses: A Literature Review. Part I -- Subcutaneous Myco¬ses. Actas Dermosifiliogr. 2016;107(10):806-15. doi: 10.1016/j.ad.2016.05.017.
12. Kauffman CA. Endemic Mycoses: Blastomy¬cosis, Histoplasmosis, and Sporotrichosis. In¬fect Dis Clin N Am. 2006;20(3):645-62. doi: 10.1016/j.idc.2006.07.002.
13. Cohen BE, Nagler AR, Pomeranz MK. Nonbac¬terial Causes of Lymphangitis with Streaking. J Am Board Fam Med. 2016;29(6):808-12. doi: 10.3122/jabfm.2016.06.160015.
14. Yang Hsu L, Wijaya L, Shu-Ting Ng E, Gotuzzo E. Tropical Fungal Infections. Infect Dis Clin NA. 2012;26(2):497-512. doi: 10.1016/j.idc.2012.02.004.
15. Hay R. Superficial fungal infec¬tions. 2017;45(11):707-10. doi: https://doi.org/10.1016/j.mpmed.2017.08.006.
16. Ampel NM. Coccidioidomycosis: A Review of Recent Advances. Clin Chest Med. 2009;30(2):241-51. doi: 10.1016/j.ccm.2009.02.004.
17. Wilson JW, Smith CE, Plunkett OA. Primary cutane¬ous coccidioidomycosis; the criteria for diagnosis and a report of a case. Calif Med. 1953;79(3):233-9.
18. Garcia Garcia SC, Salas Alanis JC, Flores MG, Gonza¬lez Gonzalez SE, Vera Cabrera L, Ocampo Candiani J. Coccidioidomycosis and the skin: a comprehensive review. An Bras Dermatol. 2015;90(5):610-21. doi: http://dx.doi.org/10.1590/abd1806-4841.20153805.
19. Bonifaz A, Tirado-Sánchez A, González GM. Cu¬taneous Coccidioidomycosis with Tissue Arthro¬conidia. Am J Trop Med Hyg. 2019;100(4):772. doi: 10.4269/ajtmh.18-0700.
20. Tortorano AM, Carminati G, Tosoni A, Tint¬elnot K. Primary Cutaneous Coccidioido¬mycosis in an Italian Nun Working in South America and Review of Published Literature. Mycopathologia. 2015;180(3-4):229-35. doi: 10.1007/s11046-015-9895-0.
21. Chang A, Tung RC, McGillis TS, Bergfeld WF, Taylor JS. Primary cutaneous coccidioidomyco¬sis. J Am Acad Dermatol. 2003;49(5):944-9. doi: 10.1016/s0190-9622(03)00462-6.
22. Dworak DP, Kapustiak J, Ehklassi TA, Patri¬anakos TD. Primary Cutaneous Coccidioido¬mycosis of the Eyelid: A Case Report. Oph-thal Plast Reconstr Surg. 2016;32(2):e40-1. doi: 10.1097/IOP.0000000000000224.
23. Baumgardner DJ, Buggy BP, Mattson BJ, Burdick JS, Ludwing D. Epidemiology of blastomycosis in a region of high endemicity in North Central Wisconsin. Clin Infect Dis. 1992;15(4):629-35. doi: 10.1093/clind/15.4.629.
24. Mcbride JA, Gauthier GM, Klein BS. Clinical Manifestations and Treatment of Blastomy¬cosis. Clin Chest Med. 2017;38(3):435-49. doi: 10.1016/j.ccm.2017.04.006.
25. Zampogna JC, Hoy MJ, Ramos-Caro FA. Pri¬mary Cutaneous North American Blasto¬mycosis in an Immunosuppressed Child. Pediatr Dermatol. 2003;20(2):128-30. doi: 10.1046/j.1525-1470.2003.20206.x.
26. Ladizinski B, Joy N, Reid DC. Primary Cutaneous Blastomycosis After Inoculation From A Woodwork¬ing Blade. J Emerg Med. 2018;54(1):e11-e12. doi: 10.1016/j.jemermed.2017.09.034.
27. Emer JJ, Spear JB. Primary cutaneous blastomy¬cosis as a cause of acute respiratory distress syn¬drome: case report and literature review. J Clin Aesthet Dermatol. 2009;2(3):22-30.
28. Mason AR, Cortes GY, Cook J, Maize JC, Thiers BH. Cutaneous blastomycosis: a diagnostic chal¬lenge. Int J Dermatol. 2008;47(8):824-30. doi: 10.1111/j.1365-4632.2008.03732.x.
29. Queiroz-Telles F, de Hoog S, Santos DWCL, Salgado CG, Vicente VA, Bonifaz A, Roi¬lides E, Xi L, Silva CMPE, Batista da Silva M, Pana ZD, Lopes A, et al. Chromoblastomyco¬sis. Clin Microbiol Rev. 2017;30(1):233-76. doi: 10.1128/CMR.00032-16.
30. Gezuele E, Mackinnon JE, Conti-Díaz IA. The fre¬quent isolation of Phialophora verrucosa and Phialophora pedrosoi from natural sources. Sab¬ouraudia. 1972;10(3):266-73.
31. Carrasco-Zuber JE, Navarrete-Dechent C, Boni¬faz A, Fich F, Vial-Letelier V, Berroeta-Mauriz¬iano D. Cutaneous involvement in the Deep Mycoses: A Review. Part II -- Systemic Mycoses. Actas Dermosifiliogr. 2016;107(10):816-22. doi: 10.1016/j.ad.2016.06.001.
32. Queiróz AJR, Pereira Domingos F, Antônio JR. Chro¬moblastomycosis: clinical experience and review of literature. Int J Dermatol. 2018;57(11):1351-5. doi: 10.1111/ijd.14185.
33. Bonifaz A, Vázquez-González D, Perusquía-Ortíz AM. Subcutaneous mycoses: chromoblastomy¬cosis, sporotrichosis and mycetoma. J Dtsch Dermatol Ges. 2010;8(8):619-27; quiz 628. doi: 10.1111/j.1610-0387.2010.07453.x.
34. Torres-Guerrero E, Isa-Isa R, Isa M, Arenas R. Chromo¬blastomycosis. Clin Dermatol. 2012;30(4):403-8. doi: 10.1016/j.clindermatol.2011.09.011.
35. de Brito AC, Bittencourt MJS. Chromoblas¬tomycosis: an etiological, epidemiological, clinical, diagnostic, and treatment update. An Bras Dermatol. 2018;93(4):495-506. doi: 10.1590/abd1806-4841.20187321.
36. Nayyar E, Taimur S. Sporotrichoid lesions: An age-old conundrum. Am J Med. 2015;128(10):e11-3. doi: 10.1016/j.amjmed.2015.04.028.
37. Sheffer S, Shreberk-Hassidim R, Olshtain K, Maly A, Zlotorgoski A, Ramot Y. Lympho¬cutaneous nocardiosis caused by Nocardia brasiliensis in an immunocompetent elderly woman. Int J Dermatol. 2016;55(1):45-7. doi: 10.1111/ijd.12988.
38. Outhred AC, Watts MR, Chen SC, Sor¬rell TC. Nocardia Infections of the Face and Neck. 2011;13(2):132-40. doi: 10.1007/s11908-011-0165-0.
39. Shahapur PR, Peerapur BV, Shahapur RP, Honnuta¬gi RM, Biradar MS. Lymphocutaneous nocardiosis caused by Nocardia otitidiscaviarum: A case report and review of literature. 2014;8(1):197-201. doi: 10.4103/0976-9668.127328.
40. Tariq EF, Anwar MM, Khan UA. Primary Cu¬taneous Nocardiosis: A Rare Presentation of Nocardiosis. Cureus. 2019;11(10):e5860. doi: 10.7759/cureus.5860.
41. Ercibengoa M, Vicente D, Arranz L, Ugarte A, Mari¬mon J. Primary Cutaneous Nocardia brasiliensis in a Spanish Child. Clin Lab. 2018;64(10):1769-72. doi: 10.7754/Clin.Lab.2018.180531.
42. Downey C, Navajas L, Andino R, Vera-kellet C, Manríquez JJ. Tuberculosis en patrón esporotri¬coide: una presentación inusual de tuberculosis cutánea en un paciente inmunocompetente. Rev. chil. infectol. 2015;32(2):234-7. doi: http://dx.doi.org/10.4067/S0716-10182015000300015.
43. Maheshwari A, Tiwari S, Mathur DK, Bhargava P. Sporotrichoid lupus vulgaris: A rare presentation. Indian Dermatol Online J. 2015;6(2):120-1. doi: 10.4103/2229-5178.153017.
44. 44. Dias MFRG, Bernardes Filho F, Qua¬resma MV, do Nascimento LV, Nery JAC, Azu¬lay DR. Update on cutaneous tuberculosis. An Bras Dermatol. 2014;89(6):925-38. doi: 10.1590/abd1806-4841.20142998.
45. Remenyik E, Nagy B, Kiss M, Veres I, Sápy M, Horkay I, Erdei I, Hunyadi J. Sporotrichoid cuta¬neous Mycobacterium tuberculosis infection in a child. Acta Derm Venereol. 2005;85(4):375-6. doi: 10.1080/00015550510030096.
46. Satoshi N, Hashimoto Y, Nishi K, Takahashi H, Takeda K, Mizumoto T, Iizuka H. Cutaneous tu¬berculosis simulating lymphocutaneous sporotri¬chosis. Australas J Dermatol. 2012;4(53):316-7. doi: 10.1111/j.1440-0960.2012.00957.x.
47. Ramesh V. Sporotrichoid cutaneous tuberculo¬sis. Clin Exp Dermatol. 2007;32(6):680-2. doi: 10.1111/j.1365-2230.2007.02481.x.
48. Premalatha S, Rao NR, Somasundaram V, Razack EA, Muthuswami T. Tuberculous Gumma in Sporotri¬choid Pattern. Int J Dermatol. 1987;26(9):600-1. doi: 10.1111/j.1365-4362.1987.tb02316.x.
49. Almaguer-Chávez J, Ocampo-Candiani J, Rendón A. [Current panorama in the diagnosis of cu¬taneous tuberculosis]. Actas Dermosifiliogr. 2009;100(7):562-70.
50. Lewis FMT, Marsh BJ, von Reyn CF. Fish Tank Exposure and Cutaneous Infections Due to Mycobacterium marinum: Tubercu¬lin Skin Testing, Treatment, and Preven¬tion. Clin Infect Dis. 2003;37(3):390-7. doi: 10.1086/376628.
51. Tirado Sánchez A, Díaz Molina VL, Morales Peña N, Bonifaz Trujillo A, Ponce Olivera MP. Granu¬loma de las peceras (piscinas). Comunicación de tres casos. Dermatología Rev Mex. 2009;53(3):150-2.
52. Belić M, Milijović J, Marko PB. Sporotrichoid pre¬sentation of Mycobacterium marinum infection of the upper extremity. A case report. 2006;15(3):135-9.
53. Hashish E, Merwad A, Elgaml S, Amer A, Ka¬mal H, Elsadek A, Marei A, Sitohy M. Myco¬bacterium marinum infection in fish and man: epidemiology, pathophysiology and manage¬ment; a review. Vet Q. 2018;38(1):35-46. doi: 10.1080/01652176.2018.1447171.
54. Alcaide F, Esteban J. Infecciones cutáneas y de partes blandas por micobacterias no tuberculosas. Enferm Infecc Microbiol Clin. 2010;28(Supl. 1):46-50. doi: 10.1016/S0213-005X(10)70008-2.
55. Orrin E, Worsnop F, Natkunarajah J. Spo¬rotrichoid Mycobacterium chelonae. Aus¬tralas J Dermatol. 2016;57(3):244-5. doi: 10.1111/ajd.12327.
56. Doudier B, Quiles-Tsimaratos N, Arniaud D. Sporotrichoid non-tuberculous mycobac¬terial infections following anti-TNF treat-ment. Med Mal Infect. 2018;48(3):222-5. doi: 10.1016/j.medmal.2017.12.006.
57. Kemp DM, Govind AG, Kang J, Brugger CC, Kauh YC. Sporotrichoid-Like Spread of Cu¬taneous Mycobacterium chelonae in an Im¬munocompromised Patient. Case Rep Dermatol Med. 2017;2017:8219841. doi: 10.1155/2017/8219841.
58. Alvar J, Vélez ID, Bern C, Herrero M, Des¬jeux P, Cano J, Jannin J, den BOer M, WHO Leishmaniasis Control Team. Leishmani¬asis Worldwide and Global Estimates of Its Incidence. PLoS One. 2012;7(5):e35671. doi: 10.1371/journal.pone.0035671.
59. Dermatología Clínica: conceptos básicos. Tamayo Buendía MM (editor). Bogotá: Centro Dermatologi¬co Federico Lleras; 2015. p. 200.
60. Calvopiña Hinojosa M, Romero Alvarez D, Kato H, Hashiguchi Y. Lesión cutánea es¬porotricoide en un paciente proceden¬te de una región subtropical de Ecuador. Enferm Infecc Microbiol Clin. 2014;32(7):465-6. doi: 10.1016/j.eimc.2014.02.007.
61. Martins Veloso de Carvalho L, Fernandes Pimentel MI, Conceicao-Silva F, de Camargo Ferreira e Vas¬concellos E, Valete-Rosalino CM, Rosandiski Lyra M, de Matos Salgueiro M, Naoto Saheki M, Madei¬ra MF, Mouta-Confort E, de Fátima Antonio L, Fa¬gundes da Silva A, et al. Sporotrichoid leishmani¬asis: a cross-sectional clinical, epidemiological and laboratory study in Rio de Janeiro State, Bra¬zil. Rev Inst Med Trop Sao Paulo. 2017;59:33. doi: 10.1590/S1678-9946201759033.
62. Kaye P, Scott P. Leishmaniasis: complex¬ity at the host–pathogen interface. Nat Rev Microbiol. 2011;9(8):604-15. doi: 10.1038/nrmicro2608.
63. Meireles CB, Maia LC, Soares GC, Teodoro IPP, Gadel¬ha M do SV, da Silva CGL, Pereira de Lima MA. Atyp¬ical presentations of cutaneous leishmaniasis: A systematic review. Acta Trop. 2017;172:240-54. doi: 10.1016/j.actatropica.2017.05.022.
64. Benzaquen M, Chambelland A, Fongue J, Melenotte C, Christen J, Ranque S, Buono JP, Parola P, Berbis P. Cutaneous sporotri¬choid leishmaniasis treated with oral flucon¬azole. Dermatol Ther. 2019;32(4):e12976. doi: 10.1111/dth.12976.
65. Rodríguez G, Arenas C, Ovalle C, Hernández CA, Camargo C. Clínica: leishmaniasis mucosas. En: Las leishmaniasis: atlas y texto. Bogotá: Hospital Universitario Centro Dermatológico Federico Lle¬ras Acosta; 2016. p. 102-11.
66. Masmoudi A, Ayadi N, Khabir A, Bouzid L, Bouas¬sida S, Meziou TJ, Akrout F, Zahaf A, Boudawara T, Turki H. Forme sporotrichoïde de leishmaniose cutanée en Tunisie: étude clinique et histologique. Ann Dermatol Venereol. 2008;135(1):63-7. doi: 10.1016/j.annder.2007.04.005.
67. Rodríguez G, Arenas C, Ovalle C, Hernández CA, Camargo C. Clínica: leishmaniasis según local¬ización. En: Las leishmaniasis: atlas y texto. Bogo¬tá: Hospital Universitatorio Centro Dermatológico Federico Lleras Acosta; 2016. p. 90-102.
How to Cite
Downloads
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2020 Revista de la Asociación Colombiana de Dermatología y Cirugía Dermatológica

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |






