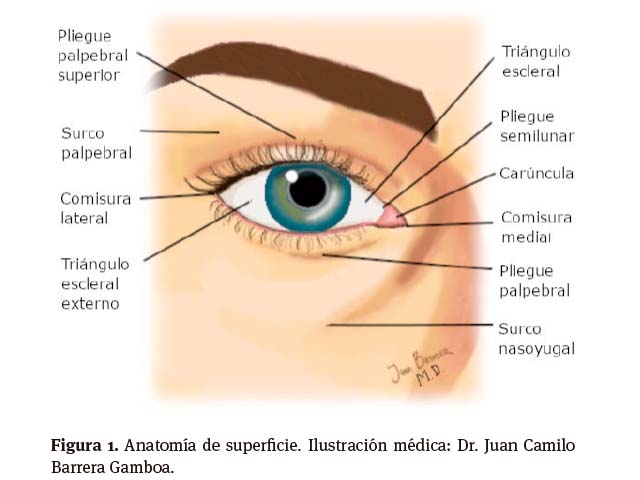
Anatomía de la órbita: estructuras en detalle y zonas de riesgo para procedimientos en la práctica dermatológica
DOI:
https://doi.org/10.29176/2590843X.1666Palabras clave:
Ácido hialurónico, Anatomía, Complicaciones, Órbita, Toxina botulínicaResumen
El conocimiento preciso de la anatomía de la órbita es importante para la realización de procedimientos quirúrgicos y no quirúrgicos o mínimamente invasivos en dermatología.
Al ser una región facial con una red vascular compleja, dependiente del sistema carotídeo externo e interno, debe ser abordada de forma cautelosa, teniendo en cuenta las zonas de riesgo para complicaciones.
Biografía del autor/a
Alejandra Toquica, Clínica de Piel – Grupo Dermatología Oncológica. Instituto Nacional de Cancerología, Bogotá, Colombia.
Clínica de Piel – Grupo Dermatología Oncológica. Instituto Nacional de Cancerología, Bogotá, Colombia.
Juan Camilo Barrera, Profesor Titular del Departamento de Medicina Interna. Universidad Nacional de Colombia, Bogotá, Colombia.
Profesor Titular del Departamento de Medicina Interna. Universidad Nacional de Colombia, Bogotá, Colombia.
Álvaro Acosta, Profesor Titular del Departamento de Medicina Interna. Universidad Nacional de Colombia, Bogotá, Colombia. Clínica de Piel – Grupo Dermatología Oncológica. Instituto Nacional de Cancerología, Bogotá, Colombia.
Profesor Titular del Departamento de Medicina Interna. Universidad Nacional de Colombia, Bogotá, Colombia. Clínica de Piel – Grupo Dermatología Oncológica. Instituto Nacional de Cancerología, Bogotá, Colombia.
Referencias bibliográficas
Sun MT, Wu A, Figueira E, Huilgol S, Selva D. Management of periorbital basal cell carcinoma with orbital invasion. Future Oncol. 2015;11(22):3003-10. https://doi.org/10.2217/fon.15.190
Iuliano A, Strianese D, Uccello G, Diplomatico A, Tebaldi S, Bonavolontà G. Risk factors for orbital exenteration in periocular Basal cell carcinoma. Am J Ophthalmol. 2012;153(2):238-41.e1. https://doi.org/10.1016/j.ajo.2011.08.004
Furdova A, Lukacko P. Periocular Basal Cell Carcinoma Predictors for Recurrence and Infiltration of the Orbit. J Craniofac Surg. 2017;28(1):e84-e7. https://doi.org/10.1097/SCS.0000000000003242
McCord, CD CM (editores). Eyelid and periorbital surgery. 2.a edición. Nueva York, Estados Unidos: Thieme Medical Publishers, Inc.; 2016.
Neimkin MG, Holds JB. Evaluation of Eyelid Function and Aesthetics. Facial Plast Surg Clin North Am. 2016;24(2):97-106. https://doi.org/10.1016/j.fsc.2015.12.002
George RM, Singer R. The lines and grooves of the face: a suggested nomenclature. Plast Reconstr Surg. 1993;92(3):540-2. https://doi.org/10.1097/00006534-199309000-00027
Frieberg T. [Participation of the lacrimal sac and lacrimal caruncle in the mechanism of lacrimation]. Ophthalmologica. 1951;122(4):193-206. https://doi.org/10.1159/000301061
Van Cruchten S, Vrolyk V, Perron Lepage MF, Baudon M, Voute H, Schoofs S, et al. Pre- and Postnatal Development of the Eye: A Species Com parison. Birth Defects Res. 2017;109(19):1540-67. https://doi.org/10.1002/bdr2.1100
Ha RY, Nojima K, Adams WP, Brown SA. Analysis of facial skin thickness: defining the relative thickness index. Plast Reconstr Surg. 2005;115(6):1769-73. https://doi.org/10.1097/01.prs.0000161682.63535.9b
Kim YS, Hwang K. Shape and Height of Tarsal Plates. J Craniofac Surg. 2016;27(2):496-7. https://doi.org/10.1097/SCS.0000000000002369
Mojallal A, Cotofana S. Anatomy of lower eyelid and eyelid-cheek junction. Ann Chir Plast Esthet. 2017;62(5):365-74. https://doi.org/10.1016/j.anplas.2017.09.007
Putterman AM, Urist MJ. Surgical anatomy of the orbital septum. Ann Ophthalmol. 1974;6(3):290-4.
Ng SK, Chan W, Marcet MM, Kakizaki H, Selva D. Levator palpebrae superioris: an anatomical update. Orbit. 2013;32(1):76-84. https://doi.org/10.3109/01676830.2012.736602
Putterman AM, Urist MJ. Müller muscle-conjunctiva resection. Technique for treatment of blepharoptosis. Arch Ophthalmol. 1975;93(8):619-23. https://doi.org/10.1001/archopht.1975.01010020595007
Kanagalingam S, Miller NR. Horner syndrome: clinical perspectives. Eye Brain. 2015;7:35-46. https://doi.org/10.2147/EB.S63633
Kakizaki H, Zhao J, Nakano T, Asamoto K, Zako M, Iwaki M, et al. The lower eyelid retractor consists of definite double layers. Ophthalmology. 2006;113(12):2346-50. https://doi.org/10.1016/j.ophtha.2006.06.017
Hwang SH, Hwang K, Jin S, Kim DJ. Location and nature of retro-orbicularis oculus fat and suborbicularis oculi fat. J Craniofac Surg. 2007;18(2):387-90. https://doi.org/10.1097/scs.0b013e31802e2a70
Leatherbarrow B, Jones PF. Oculoplastic Surgery. 3.a edición. Nueva York, Estados Unidos: Thieme Medical Publishers Inc.; 2019.
Chen W. Occuloplastic Surgery. The Essentials. Nueva York, Estados Unidos: Thieme Medical Publishers; 2001.
Levine MR, Allen RC. Manual of Oculoplastic Surgery. 5.a edición. Springer International Publishing; 2018.
Hwang K, Joong Kim D, Chung RS. Pretarsal fat compartment in the lower eyelid. Clin Anat. 2001;14(3):179-83. https://doi.org/10.1002/ca.1030
Sires BS, Lemke BN, Dortzbach RK, Gonnering RS. Characterization of human orbital fat and connective tissue. Ophthalmic Plast Reconstr Surg. 1998;14(6):403-14. https://doi.org/10.1097/00002341-199811000-00004
Kruglikov I, Trujillo O, Kristen Q, Isac K, Zorko J, Fam M, et al. The Facial Adipose Tissue: A Revision. Facial Plast Surg. 2016;32(6):671-82. https://doi.org/10.1055/s-0036-1596046
Cotofana S, Lachman N. Anatomy of the Facial Fat Compartments and their Relevance in Aesthetic Surgery. J Dtsch Dermatol Ges. 2019;17(4):399-413. https://doi.org/10.1111/ddg.13737
Ghavami A, Pessa JE, Janis J, Khosla R, Reece EM, Rohrich RJ. The orbicularis retaining ligament of the medial orbit: closing the circle. Plast Reconstr Surg. 2008;121(3):994-1001. https://doi.org/10.1097/01.prs.0000299941.62645.4e
Erdogmus S, Govsa F. The arterial anatomy of the eyelid: importance for reconstructive and aesthetic surgery. J Plast Reconstr Aesthet Surg. 2007;60(3):241-5. https://doi.org/10.1016/j.bjps.2006.01.056
Cotofana S, Lachman N. Arteries of the Face and Their Relevance for Minimally Invasive Facial Procedures: An Anatomical Review. Plast Reconstr Surg. 2019;143(2):416-26. https://doi.org/10.1097/PRS.0000000000005201
Cotofana S, Steinke H, Schlattau A, Schlager M, Sykes JM, Roth MZ, et al. The Anatomy of the Facial Vein: Implications for Plastic, Reconstructive, and Aesthetic Procedures. Plast Reconstr Surg. 2017;139(6):1346-53. https://doi.org/10.1097/PRS.0000000000003382
Echegoyen JC, Hirabayashi KE, Lin KY, Tao JP. Imaging of eyelid lymphatic drainage. Saudi J Ophthalmol. 2012;26(4):441-3. https://doi.org/10.1016/j.sjopt.2012.08.003
Munger BL, Halata Z. The sensorineural apparatus of the human eyelid. Am J Anat. 1984;170(2):181-204. https://doi.org/10.1002/aja.1001700205
Lowe JB, Cohen M, Hunter DA, Mackinnon SE. Analysis of the nerve branches to the orbicularis oculi muscle of the lower eyelid in fresh cadavers. Plast Reconstr Surg. 2005;116(6):1743-9; discussion 50-1. https://doi.org/10.1097/01.prs.0000186532.29557.96
Reciente estudio internacional muestra que la cirugía estética continúa aumentando en todo el mundo [Internet]. International Society of Aesthetic Plastic Surgery; 2018; Disponible en: https://bit.ly/3FWLu5q
Urdiales-Gálvez F, Delgado NE, Figueiredo V, LajoPlaza JV, Mira M, Ortíz-Martí F, et al. Preventing the Complications Associated with the Use of Dermal Fillers in Facial Aesthetic Procedures: An Expert Group Consensus Report. Aesthetic Plast Surg. 2017;41(3):667-77. https://doi.org/10.1007/s00266-017-0798-y
Stroman DW, Mintun K, Epstein AB, Brimer CM, Patel CR, Branch JD, et al. Reduction in bacterial load using hypochlorous acid hygiene solution on ocular skin. Clin Ophthalmol. 2017;11:707-14. https://doi.org/10.2147/OPTH.S132851
Murthy R, Roos JCP, Goldberg RA. Periocular hyaluronic acid fillers: applications, implications, complications. Curr Opin Ophthalmol. 2019;30(5):395-400. https://doi.org/10.1097/ICU.0000000000000595
DeLorenzi C. Complications of injectable fillers, part I. Aesthet Surg J. 2013;33(4):561-75. https://doi.org/10.1177/1090820X13484492
Funt D, Pavicic T. Dermal fillers in aesthetics: an overview of adverse events and treatment approaches. Clin Cosmet Investig Dermatol. 2013;6:295-316. https://doi.org/10.1177/1090820X13484492
Hirsch RJ, Narurkar V, Carruthers J. Management of injected hyaluronic acid induced Tyndall effects. Lasers Surg Med. 2006;38(3):202-4. https://doi.org/10.1002/lsm.20283
Skippen B, Baldelli I, Hartstein M, Casabona G, Montes JR, Bernardini F. Rehabilitation of the Dysmorphic Lower Eyelid From Hyaluronic Acid Filler: What to Do After a Good Periocular Treatment Goes Bad. Aesthet Surg J. 2020;40(2):197-205. https://doi.org/10.1093/asj/sjz078
Wijemanne S, Vijayakumar D, Jankovic J. Apraclonidine in the treatment of ptosis. J Neurol Sci. 2017;376:129-32. https://doi.org/10.1016/j.jns.2017.03.025
Wutthiphan S, Kowal L, O'Day J, Jones S, Price J. Diplopia following subcutaneous injections of botulinum A toxin for facial spasms. J Pediatr Ophthalmol Strabismus. 1997;34(4):229-34.
Lee SK, Jun HJ. Esotropia following botulinum toxin type A injection for facial wrinkles. J Cosmet Laser Ther. 2018;20(1):50-1. https://doi.org/10.1080/14764172.2017.1349322
Hsu TS, Dover JS, Arndt KA. Effect of volumen and concentration on the diffusion of botulinum exotoxin A. Arch Dermatol. 2004;140(11):1351-4. https://doi.org/10.1001/archderm.140.11.1351
Rzany B, DeLorenzi C. Understanding, Avoiding, and Managing Severe Filler Complications. Plast Reconstr Surg. 2015;136(5 Suppl):196S-203S. https://doi.org/10.1097/PRS.0000000000001760
Weinberg MJ, Solish N. Complications of hyaluronic acid fillers. Facial Plast Surg. 2009;25(5):324-8. https://doi.org/10.1055/s-0029-1243081
DeLorenzi C. New High Dose Pulsed Hyaluronidase Protocol for Hyaluronic Acid Filler Vascular Adverse Events. Aesthet Surg J. 2017;37(7):814-25. https://doi.org/10.1093/asj/sjw251
Goodman GJ, Clague MD. A Rethink on Hyaluronidase Injection, Intraarterial Injection, and Blindness: Is There Another Option for Treatment of Retinal Artery Embolism Caused by Intraarterial Injection of Hyaluronic Acid? Dermatol Surg. 2016;42(4):547-9. https://doi.org/10.1097/dss.0000000000000670
Cómo citar
Descargas
Descargas
Publicado
Cómo citar
Número
Sección

| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |






