Reacciones adversas medicamentosas cutáneas: enfoque en el servicio de urgencias
DOI:
https://doi.org/10.29176/2590843X.1728Palabras clave:
Erupciones por medicamentos, Necrólisis epidérmica tóxica, Síndrome de hipersensibilidad a medicamentos, Síndrome de Stevens-JohnsonResumen
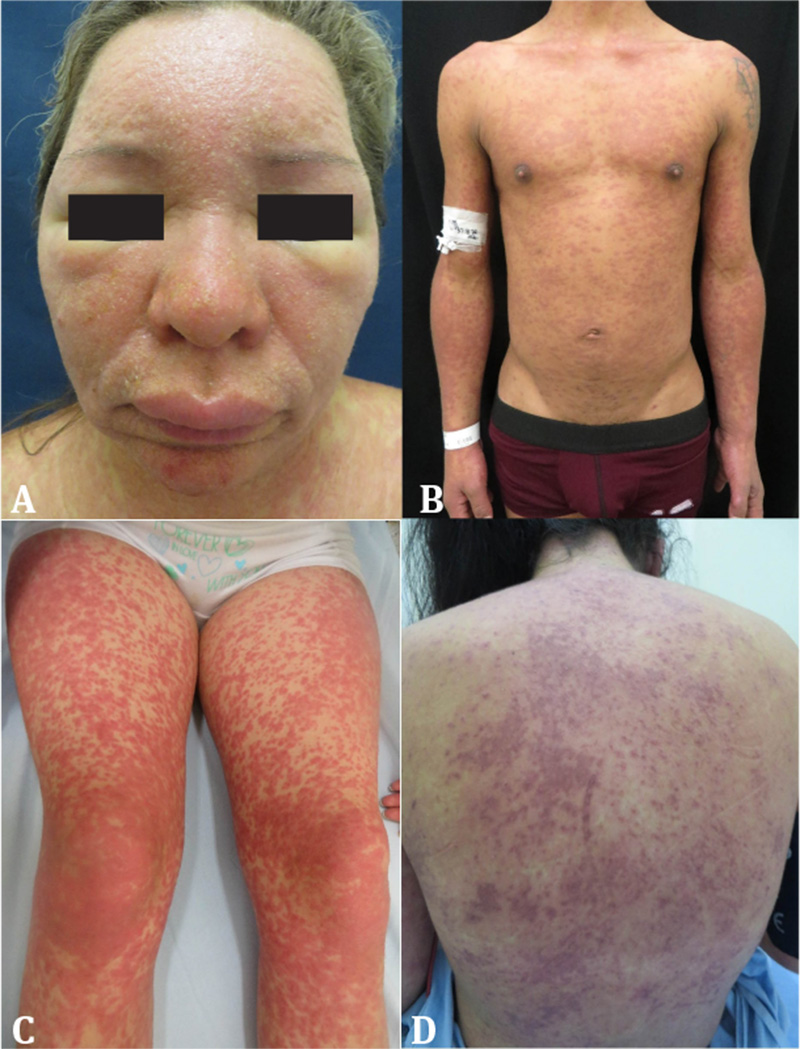
Las erupciones cutáneas están dentro de las reacciones adversas medicamentosas más frecuentes; por lo tanto, es habitual enfrentarse a estas en los diferentes ámbitos del ejercicio médico. Un enfoque ordenado basado en la identificación temprana del posible agente etiológico, la cronología de la exposición y las características clínicas de la reacción permiten categorizar la gravedad del cuadro. Con una sospecha clara puede optimizarse la toma de paraclínicos, elegirse el nivel de complejidad asistencial más adecuado y tomarse las medidas terapéuticas y preventivas pertinentes para cada caso. En la siguiente revisión narrativa se pretende abarcar los aspectos clave de las erupciones medicamentosas más graves y proponer un enfoque simple de estas en el servicio de urgencias.
Referencias bibliográficas
Shear N, Knowles S. Cutaneus Reactions to Drugs. En: Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell D, Wolff K (editores). Fitzpatrick’s Dermatology in General Medicine. 8.a edición. Estados Unidos: McGraw-Hill; 2012.
Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA. 1998;279(15):1200-5. https://doi.org/10.1001/jama.279.15.1200
Organización Mundial de la Salud. Formulario Modelo de la OMS 2004: Consejo general a los prescriptores: Efectos adversos e interacciones. Disponible en: https://bit.ly/3a3XuGH
Trujillo MC, Vásquez LA. Características clínicas y epidemiológicas de las toxicodermias en pacientes hospitalizados del Hospital Pablo Tobón Uribe, Medellín, Colombia, 2007-2009. Rev Asoc Colomb Dermatol. 2012;20(3):231-6. https://doi.org/10.29176/2590843X.234
Zhang J, Zixian L, Xu C, Zhao J, Kang X. Current Perspectives on Severe Drug Eruption. Clin Rev Allergy Immunol. 2021;61(3):1-17. https://doi.org/10.1007/s12016-021-08859-0
Bigby M. Rates of cutaneous reactions to drugs. Arch Dermatol. 2001;137(6):765-70.
Bolognia JL, Jorizzo JL, Schaffer JV (editores). Bolognia. Dermatología: Principales diagnósticos y tratamientos. España: Elsevier; 2015.
Khan D, Solensky R. Drug allergy. J Allergy Clin Immunol. 2010;125(2 Suppl 2):S126-137. https://doi.org/10.1016/j.jaci.2009.10.028
Romano A, Pettinato R, Andriolo M, Viola M, Guéant-Rodriguez R-M, Valluzzi RL, et al. Hypersensitivity to aromatic anticonvulsants: in vivo and in vitro cross-reactivity studies. Curr Pharm Des. 2006;12(26):3373-81. https://doi.org/10.2174/138161206778193962
Maniu C-M, Buss G, Feldmeyer L, Spertini F, Ribi C. [Severe delayed drug hypersensitivity reactions]. Rev Med Suisse. 2013;9(382):803-4, 806-11.
Celik G, Pichler WJ, Adkinson NF Jr. Drug Allergy. En: Adkinson NF, Middleton E (editores). Middleton's Allergy Principles & Practice. 7.a edi ción. Filadelfia: Mosby Elsevier; 2009. p.1205-26.
Hung SI, Chung WH, Jee SH, Chen WC, Chang YT, Lee WR, et al. Genetic susceptibility to carbamazepine-induced cutaneous adverse drug reactions. Pharmacogenet Genomics. 2006;16(4):297-306. https://doi.org/10.1097/01.fpc.0000199500.46842.4a
Dainichi T, Uchi H, Moroi Y, Furue M. StevensJohnson syndrome, drug-induced hypersensitivity syndrome and toxic epidermal necrolysis caused by allopurinol in patients with a common HLA allele: what causes the diversity? Dermatology. 2007;215(1):86-8. https://doi.org/10.1159/000102045
Tozzi V. Pharmacogenetics of antiretrovirals. Antivir Res. 2010;85(1):190-200. https://doi.org/10.1016/j.antiviral.2009.09.001
Musette P, Janela B. New Insights into Drug Reaction with Eosinophilia and Systemic Symptoms Pathophysiology. Front Med (Lausanne). 2017;4:179. https://doi.org/10.3389/fmed.2017.00179
Tempark T, Satapornpong P, Rerknimitr P, Nakkam N, Saksit N, Wattanakrai P, et al. Dapsone-induced severe cutaneous adverse drug reactions are strongly linked with HLA-B*13: 01 allele in the Thai population. Pharmacogenet Genomics. 2017;27(12):429-37. https://doi.org/10.1097/FPC.0000000000000306
McCormack M, Alfirevic A, Bourgeois S, Farrell JJ, Kasperavičiūtė D, Carrington M, et al. HLAA*3101 and carbamazepine-induced hypersensitivity reactions in Europeans. N Engl J Med. 2011;364(12):1134-43. https://doi.org/10.1056/NEJMoa1013297
Uetrecht JP. Is it possible to more accurately predict which drug candidates will cause idiosyncratic drug reactions? Curr Drug Metab. 2000;1(2):133-41. https://doi.org/10.2174/1389200003339081
Seishima M, Yamanaka S, Fujisawa T, Tohyama M, Hashimoto K. Reactivation of human herpesvirus (HHV) family members other than HHV-6 in druginduced hypersensitivity syndrome. Br J Dermatol. 2006;155(2):344-9. https://doi.org/10.1111/j.1365-2133.2006.07332.x
Ben m’rad M, Leclerc-Mercier S, Blanche P, Franck N, Rozenberg F, Fulla Y, et al. Drug-induced hypersensitivity syndrome: clinical and biologic disease patterns in 24 patients. Medicine (Baltimore). 2009;88(3):131-40. https://doi.org/10.1097/MD.0b013e3181a4d1a1
Chiou C-C, Yang L-C, Hung S-I, Chang Y-C, Kuo T-T, Ho H-C, et al. Clinicopathological features and prognosis of drug rash with eosinophilia and systemic symptoms: a study of 30 cases in Taiwan. J Eur Acad Dermatol Venereol. 2008;22(9):1044-9. https://doi.org/10.1111/j.1468-3083.2008.02585.x
Ding WY, Lee CK, Choon SE. Cutaneous adverse drug reactions seen in a tertiary hospital in Johor, Malaysia. Int J Dermatol. 2010;49(7):834-42. https://doi.org/10.1111/j.1365-4632.2010.04481.x
Häusermann P, Harr T, Bircher AJ. Baboon syndrome resulting from systemic drugs: is there strife between SDRIFE and allergic contact dermatitis syndrome? Contact Dermatitis. 2004;51(5-6):297-310. https://doi.org/10.1111/j.0105-1873.2004.00445.x
Swanson L, Colven RM. Approach to the Patient with a Suspected Cutaneous Adverse Drug Reaction. Med Clin North Am. 2015;99(6):1337-48. https://doi.org/10.1016/j.mcna.2015.06.003
Inamadar AC, Palit A. Acute skin failure: concept, causes, consequences and care. Indian J Dermatol Venereol Leprol. 2005;71(6):379-85. https://doi.org/10.4103/0378-6323.18007
Merritt HH, Putnam TJ. Sodium diphenyl hydantoinate in the treatment of convulsive disorders. J Am Med Assoc. 1938;111(12):1068-73.
Bocquet H, Bagot M, Roujeau JC. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (Drug Rash with Eosinophilia and Systemic Symptoms: DRESS). Semin Cutan Med Surg. 1996;15(4):250-7. https://doi.org/10.1016/s1085-5629(96)80038-1
Husain Z, Reddy BY, Schwartz RA. DRESS syn drome: Part I. Clinical perspectives. J Am Acad Dermatol. 2013;68(5):693.e1-14; quiz 706-8. https://doi.org/10.1016/j.jaad.2013.01.033
Muller P, Dubreil P, Mahé A, Lamaury I, Salzer B, Deloumeaux J, et al. Drug Hypersensitivity Syndrome in a West-Indian population. Eur J Dermatol. 2003;13(5):478-81.
Shiohara T, Kano Y. Drug reaction with eosinophilia and systemic symptoms (DRESS): incidence, pathogenesis and management. Expert Opin Drug Saf. 2017;16(2):139-47. https://doi.org/10.1080/14740338.2017.1270940
Tennis P, Stern RS. Risk of serious cutaneous disorders after initiation of use of phenytoin, carbamazepine, or sodium valproate: a record linkage study. Neurology. 1997;49(2):542-6. https://doi.org/10.1212/wnl.49.2.542
Guberman AH, Besag FM, Brodie MJ, Dooley JM, Duchowny MS, Pellock JM, et al. Lamotrigine associated rash: risk/benefit considerations in adults and children. Epilepsia. 1999;40(7):985-91. https://doi.org/10.1111/j.1528-1157.1999.tb00807.x
Kim GY, Anderson KR, Davis DMR, Hand J, Tollefson M. Drug reaction with eosinophilia and systemic symptoms (DRESS) in the pediatric population: A systematic review of the literature. J Am Acad Dermatol. 2020;83(5):1323-30. https://doi.org/10.1016/j.jaad.2020.03.081
Mattoussi N, Mansour AB, Essadam L, Guedri R, Fitouri Z, Becher S. Drug Reaction With Eosinophilia and Systemic Symptoms (DRESS) Syndrome in Children: A Case Report. J Investig Allergol Clin Immunol. 2017;27(2):144-6. https://doi.org/10.18176/jiaci.0140
Cacoub P, Musette P, Descamps V, Meyer O, Speirs C, Finzi L, et al. The DRESS syndrome: a literature review. Am J Med. 2011;124(7):588-97. https://doi.org/10.1016/j.amjmed.2011.01.017
Kardaun SH, Sekula P, Valeyrie-Allanore L, Liss Y, Chu CY, Creamer D, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS): an original multisystem adverse drug reaction. Results from the prospective RegiSCAR study. Br J Dermatol. 2013;169(5):1071-80. https://doi.org/10.1111/bjd.12501
Kardaun SH, Sidoroff A, Valeyrie-Allanore L, Halevy S, Davidovici BB, Mockenhaupt M, et al. Variability in the clinical pattern of cutaneous side effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br J Dermatol. 2007;156(3):609-11. https://doi.org/10.1111/j.1365-2133.2006.07704.x
Ichai P, Laurent-Bellue A, Saliba F, Moreau D, Besch C, Francoz C, et al. Acute Liver Failure/Injury Related to Drug Reaction With Eosinophilia and Systemic Symptoms: Outcomes and Prognostic Factors. Transplantation. 2017;101(8):1830-7. https://doi.org/10.1097/TP.0000000000001655
Walsh S, Creamer D. Drug reaction with eosinophilia and systemic symptoms (DRESS): a clinical update and review of current thinking. Clin Exp Dermatol. 2011;36(1):6-11. https://doi.org/10.1111/j.1365-2230.2010.03967.x
Tetart F, Picard D, Janela B, Joly P, Musette P. Prolonged evolution of drug reaction with eosinophilia and systemic symptoms: clinical, virologic, and biological features. JAMA Dermatol. 2014;150(2):206-7. https://doi.org/10.1001/jamadermatol.2013.6698
Kano Y, Shiohara T. The variable clinical picture of drug-induced hypersensitivity syndrome/drug rash with eosinophilia and systemic symptoms in relation to the eliciting drug. Immunol Allergy Clin North Am. 2009;29(3):481-501. https://doi.org/10.1016/j.iac.2009.04.007
Valeyrie-Allanore L, Sassolas B, Roujeau J-C. Drug-induced skin, nail and hair disorders. Drug Saf. 2007;30(11):1011-30. https://doi.org/10.2165/00002018-200730110-00003
Bachot N, Roujeau J-C. Differential diagnosis of severe cutaneous drug eruptions. Am J Clin Dermatol. 2003;4(8):561-72. https://doi.org/10.2165/00128071-200304080-00006
Schnyder B, Pichler WJ. Mechanisms of Drug-Induced Allergy. Mayo Clin Proc. 2009;84(3):268-72. https://doi.org/10.1016/S0025-6196(11)61145-2
Uhara H, Saiki M, Kawachi S, Ashida A, Oguchi S, Okuyama R. Clinical course of drug-induced hypersensitivity syndrome treated without systemic corticosteroids. J Eur Acad Dermatol Venereol. 2013;27(6):722-6. https://doi.org/10.1111/j.1468-3083.2012.04547.x
Funck-Brentano E, Duong T-A, Bouvresse S, Bagot M, Wolkenstein P, Roujeau J-C, et al. Therapeutic management of DRESS: a retrospective study of 38 cases. J Am Acad Dermatol. 2015;72(2):246-52. https://doi.org/10.1016/j.jaad.2014.10.032
Zuliani E, Zwahlen H, Gilliet F, Marone C. Vancomycin-induced hypersensitivity reaction with acute renal failure: resolution following cyclosporine treatment. Clin Nephrol. 2005;64(2):155-8. https://doi.org/10.5414/cnp64155
Kirchhof MG, Wong A, Dutz JP. Cyclosporine Treatment of Drug-Induced Hypersensitivity Syndrome. JAMA Dermatol. 2016;152(11):1254-7. https://doi.org/10.1001/jamadermatol.2016.2220
Ushigome Y, Kano Y, Ishida T, Hirahara K, Shiohara T. Short- and long-term outcomes of 34 patients with drug-induced hypersensitivity syndrome in a single institution. J Am Acad Dermatol. 2013;68(5):721-8. https://doi.org/10.1016/j.jaad.2012.10.017
Stevens AM, Johnson FC. A new eruptive fever associated with stomatitis and ophthalmia: report of two cases in children. Am J Dis Child. 1922;24(6):526-33. https://doi.org/10.1001/archpedi.1922.04120120077005
Lyell A. Toxic epidermal necrolysis: an eruption resembling scalding of the skin. Br J Dermatol. 1956;68(11):355-61. https://doi.org/10.1111/j.1365-2133.1956.tb12766.x
Stern RS, Divito SJ. Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis: Associations, Outcomes, and Pathobiology-Thirty Years of Progress but Still Much to Be Done. J Invest Dermatol. 2017;137(5):1004-8. https://doi.org/10.1016/j.jid.2017.01.003
Paquet P, Piérard GE. New Insights in Toxic Epidermal Necrolysis ( Lyeirs Syndrome): clinical considerations, pathobiology and targeted treatments revisited. Drug Saf. 2010;33(3):189-212. https://doi.org/10.2165/11532540-000000000-00000
Rzany B, Mockenhaupt M, Baur S, Schröder W, Stocker U, Mueller J, et al. Epidemiology of erythema exsudativum multiforme majus, Stevens-Johnson syndrome, and toxic epidermal necrolysis in Germany (1990-1992): structure and results of a population-based registry. J Clin Epidemiol. 1996;49(7):769-73. https://doi.org/10.1016/0895-4356(96)00035-2
Sekula P, Dunant A, Mockenhaupt M, Naldi L, Bouwes Bavinck JN, Halevy S, et al. Comprehensive survival analysis of a cohort of patients with Stevens-Johnson syndrome and toxic epidermal necrolysis. J Invest Dermatol. 2013;133(5):1197-204. https://doi.org/10.1038/jid.2012.510
Correia O, Delgado L, Ramos JP, Resende C, Torrinha JA. Cutaneous T-cell recruitment in toxic epidermal necrolysis. Further evidence of CD8+ lymphocyte involvement. Arch Dermatol. 1993;129(4):466-8.
Nassif A, Bensussan A, Boumsell L, Deniaud A, Moslehi H, Wolkenstein P, et al. Toxic epidermal necrolysis: effector cells are drug-specific cytotoxic T cells. J Allergy Clin Immunol. 2004;114(5):1209-15. https://doi.org/10.1016/j.jaci.2004.07.047
Wei C-Y, Chung W-H, Huang H-W, Chen Y-T, Hung S-I. Direct interaction between HLA-B and carbamazepine activates T cells in patients with Stevens-Johnson syndrome. J Allergy Clin Immunol. 2012;129(6):1562-1569.e5. https://doi.org/10.1016/j.jaci.2011.12.990
Roujeau J-C, Bricard G, Nicolas J-F. Drug-induced epidermal necrolysis: Important new piece to end the puzzle. J Allergy Clin Immunol. 2011;128(6):1277-8. https://doi.org/10.1016/j.jaci.2011.10.015
Ko T-M, Chung W-H, Wei C-Y, Shih H-Y, Chen J-K, Lin C-H, et al. Shared and restricted T-cell receptor use is crucial for carbamazepine-induced Stevens-Johnson syndrome. J Allergy Clin Immunol. 2011;128(6):1266-76.e11. https://doi.org/10.1016/j.jaci.2011.08.013
Yoshioka M, Sawada Y, Nakamura M. Diagnostic Tools and Biomarkers for Severe Drug Eruptions. Int J Mol Sci. 2021;22(14):7527. https://doi.org/10.3390/ijms22147527
Chung W-H, Hung S-I, Yang J-Y, Su S-C, Huang S-P, Wei C-Y, et al. Granulysin is a key mediator for disseminated keratinocyte death in Stevens-Johnson syndrome and toxic epidermal necrolysis. Nat Med. 2008;14(12):1343-50. https://doi.org/10.1038/nm.1884
Mittmann N, Knowles SR, Koo M, Shear NH, Rachlis A, Rourke SB. Incidence of toxic epidermal necrolysis and Stevens-Johnson Syndrome in an HIV cohort: an observational, retrospective case series study. Am J Clin Dermatol. 2012;13(1):49-54. https://doi.org/10.2165/11593240-000000000-00000
Gillis NK, Hicks JK, Bell GC, Daly AJ, Kanetsky PA, McLeod HL. Incidence and Triggers of Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis in a Large Cancer Patient Cohort. J Invest Dermatol. 2017;137(9):2021-3. https://doi.org/10.1016/j.jid.2017.05.010
Sassolas B, Haddad C, Mockenhaupt M, Dunant A, Liss Y, Bork K, et al. ALDEN, an algorithm for assessment of drug causality in Stevens-Johnson Syndrome and toxic epidermal necrolysis: comparison with case-control analysis. Clin Pharmacol Ther. 2010;88(1):60-8. https://doi.org/10.1038/clpt.2009.252
Mockenhaupt M, Viboud C, Dunant A, Naldi L, Halevy S, Bouwes Bavinck J, et al. Stevens-Johnson syndrome and toxic epidermal necrolysis: assessment of medication risks with emphasis on recently marketed drugs. The EuroSCAR-study. J Invest Dermatol. 2008;128(1):35-44. https://doi.org/10.1038/sj.jid.5701033
Harr T, French LE. Toxic epidermal necrolysis and Stevens-Johnson syndrome. Orphanet J Rare Dis. 2010;5(1):39. https://doi.org/10.1186/1750-1172-5-39
Bastuji-Garin S, Fouchard N, Bertocchi M, Roujeau JC, Revuz J, Wolkenstein P. SCORTEN: a severity of-illness score for toxic epidermal necrolysis. J Invest Dermatol. 2000;115(2):149-53. https://doi.org/10.1046/j.1523-1747.2000.00061.x
Guégan S, Bastuji-Garin S, Poszepczynska-Guigné E, Roujeau J-C, Revuz J. Performance of the SCORTEN during the first five days of hospitalization to predict the prognosis of epidermal necrolysis. J Invest Dermatol. 2006;126(2):272-6. https://doi.org/10.1038/sj.jid.5700068
Cartotto R, Mayich M, Nickerson D, Gomez M. SCORTEN accurately predicts mortality among toxic epidermal necrolysis patients treated in a burn center. J Burn Care Res. 2014;29(1):141-6. https://doi.org/10.1097/BCR.0b013e31815f3865
Trent JT, Kirsner RS, Romanelli P, Kerdel FA. Use of SCORTEN to accurately predict mortality in patients with toxic epidermal necrolysis in the United States. Arch Dermatol. 2004;140(7):890-2. https://doi.org/10.1001/archderm.140.7.890
Garg T, Sanke S, Ahmed R, Chander R, Basu S. Stevens-Johnson syndrome and toxic epidermal necrolysis-like cutaneous presentation of chikungunya fever: A case series. Pediatr Dermatol. 2018;35(3):392-6. https://doi.org/10.1111/pde.13450
Dorafshar AH, Dickie SR, Cohn AB, Aycock JK, O’Connor A, Tung A, et al. Antishear therapy for toxic epidermal necrolysis: an alternative treatment approach. Plast Reconstr Surg. 2008;122(1):154-60. https://doi.org/10.1097/PRS.0b013e3181773d5d
Ng QX, De Deyn MLZQ, Venkatanarayanan N, Ho CYX, Yeo W-S. A meta-analysis of cyclosporine treatment for Stevens-Johnson syndrome/toxic epidermal necrolysis. J Inflamm Res. 2018;11:135-42. https://doi.org/10.2147/JIR.S160964
Zimmermann S, Sekula P, Venhoff M, Motschall E, Knaus J, Schumacher M, et al. Systemic Immunomodulating Therapies for Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis: A Systematic Review and Meta-analysis. JAMA Dermatol. 2017;153(6):514-22. https://doi.org/10.1001/jamadermatol.2016.5668
Mockenhaupt M. The current understanding of Stevens-Johnson syndrome and toxic epidermal necrolysis. Expert Rev Clin Immunol. 2011;7(6):803-13; quiz 814-5. https://doi.org/10.1586/eci.11.66
Finkelstein Y, Soon GS, Acuna P, George M, Pope E, Ito S, et al. Recurrence and outcomes of Stevens-Johnson syndrome and toxic epidermal necrolysis in children. Pediatrics. 2011;128(4):723-8. https://doi.org/10.1542/peds.2010-3322
Schwartz R, McDonough PH, Lee BW. Toxic epidermal necrolysis: Part II. Prognosis, sequelae, diagnosis, differential diagnosis, prevention, and treatment. J Am Acad Dermatol. 2013;69(2):187. e1-16; quiz 203-4. https://doi.org/10.1016/j.jaad.2013.05.002
Yip LW, Thong BY, Lim J, Tan a W, Wong HB, Handa S, et al. Ocular manifestations and complications of Stevens-Johnson syndrome and toxic epidermal necrolysis: an Asian series. Allergy. 2007;62(5):527-31. https://doi.org/10.1111/j.1398-9995.2006.01295.x
Meneux E, Wolkenstein P, Haddad B, Roujeau JC, Revuz J, Paniel BJ. Vulvovaginal involvement in toxic epidermal necrolysis: a retrospective study of 40 cases. Obstet Gynecol. 1998;91(2):283-7. https://doi.org/10.1016/s0029-7844(97)00596-6
Sheridan RL, Schulz JT, Ryan CM, Schnitzer JJ, Lawlor D, Driscoll DN, et al. Long-Term Consequences of Toxic Epidermal Necrolysis in Children. Pediatrics. 2002;109(1):74-8. https://doi.org/10.1542/peds.109.1.74
Atzori L, Perla S, Atzori MG, Ferreli C, Rongioletti F. Cutaneous drug eruptions associated with COVID-19 therapy. JAAD Int. 2020;1(1):73-6. https://doi.org/10.1016/j.jdin.2020.05.004
Ramirez E, Urroz M, Rodríguez A, González-Muñoz M, Martín-Vega A, Villánet Y, et al. Incidence of Suspected Serious Adverse Drug Reactions in Corona Virus Disease-19 Patients Detected by a Pharmacovigilance Program by Laboratory Signals in a Tertiary Hospital in Spain: Cautionary Data. Front Pharmacol. 2020 ;11:602841. https://doi.org/10.3389/fphar.2020.602841
Cómo citar
Descargas
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2022 Revista de la Asociación Colombiana de Dermatología y Cirugía Dermatológica

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-CompartirIgual 4.0.

| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |






