Síndromes de hipersensibilidad inducidos por medicamentos en las unidades de cuidados intensivos
DOI:
https://doi.org/10.29176/2590843X.58Palabras clave:
síndrome de Stevens-Johnson, síndrome de hipersensibilidad a medicamentos, cuidados críticos, preparaciones farmacéuticas, unidad de cuidados intensivos, erupciones cutáneasResumen
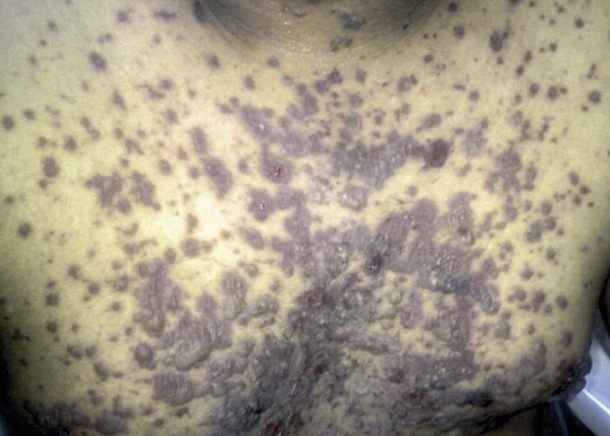
Las enfermedades cutáneas desencadenadas por medicamentos son comunes y, en su mayoría, no fatales; sin embargo, algunas de ellas menos frecuentes, son potencialmente mortales. Se destaca el espectro del síndrome de Stevens-Johnson/necrólisis epidérmica tóxica y el síndrome de hipersensibilidad a medicamentos con eosinofilia y síntomas sistémicos.
Al ser enfermedades de baja incidencia, es común que el personal de cuidados intensivos no esté familiarizado con su presentación, diagnóstico y tratamiento, lo que puede asociarse con demoras en la atención adecuada y con impacto en la
morbimortalidad.
En esta revisión narrativa se abordan estas entidades clínicas y se describe su asociación con medicamentos de uso frecuente en las unidades de cuidados intensivos; además, se tratan la fisiopatología, la presentación clínica y el tratamiento.
Biografía del autor/a
Marcela Cardona, Centro de Simulación Clínica, grupo EdSimC
Médica general, Vital Care, Centro de Simulación Clínica, grupo EdSimC, Armenia, Colombia
Luisa Fernanda Galindo, Dermobog
Médica dermatóloga, Dermobog, Bogotá, D.C., Colombia
Diego Andrés Díaz-Guío, Vital Care, Centro de Simulación
Médico intensivista, Ph.D. (c) en Educación, Clínica Central del Quindío, CEO Vital Care, Centro de Simulación, Armenia, Colombia
Referencias bibliográficas
Roujeau J. Clinical heterogeneity of drug hypersensitivity. Toxicology. 2005;209:123-9. https://doi.org/10.1016/j.tox.2004.12.022
Steven A, Johnson F. A new eruptive fever associated with stomatitis and ophthalmia. Am J Dis Child. 1922;(Case 2). https://doi.org/10.1001/archpedi.1922.04120120077005
Bohigian GM. The history of Stevens-Johnson Syndrome and a case study. Cent Hist Med Washingt Univ Sch Med St Louis [Internet]. 2015; Available from: http://digitalcommons.wustl.edu/historyofmedicine_presentations/1.
Lyell A. Toxic epidermal necrolysis: An eruption resembling scalding of the skin. Br J Dermatol. 1956;68:355-61. https://doi.org/10.1111/j.1365-2133.1956.tb12766.x
Sun J, Liu J, Gong QL, Ding GZ, Ma LW, Zhang LC, et al. Stevens-Johnson Syndrome and toxic epidermal necrolysis: A multi-aspect comparative 7-year study from the People's Republic of China. Drug Des Devel Ther. 2014;8:2539-47. https://doi.org/10.2147/DDDT.S71736
Harr T, French LE. Severe cutaneous adverse reactions: Acute generalized exanthematous pustulosis, toxic epidermal necrolysis and Stevens-Johnson syndrome. Med Clin North Am. 2010;94:727-42. https://doi.org/10.1016/j.mcna.2010.04.004
Lin YF, Yang CH, Sindy H, Lin JY, Hui CYR, Tsai YC, et al. Severe cutaneous adverse reactions related to systemic antibiotics. Clin Infect Dis. 2014;58:1377-85. https://doi.org/10.1093/cid/ciu126
Mahar PD, Wasiak J, Hii B, Cleland H, Watters DA, Gin D, et al. A systematic review of the management and outcome of toxic epidermal necrolysis treated in burns centres. Burns. 2014;40:1245-54. https://doi.org/10.1016/j.burns.2014.02.006
Badia M, Serviá L, Casanova JM, Montserrat N, Vilanova J, Vicario E, et al. Classification of dermatological disorders in critical care patients: A prospective observational study. J Crit Care. 2013;28:220.e1-220.e8. https://doi.org/10.1016/j.jcrc.2012.06.006
Peña-Hoyos ÁA. Enfermedades dermatológicas de pacientes hospitalizados en cuidados intensivos, Hospital de La Samaritana. Bogotá: Universidad Nacional de Colombia; 2016.
Victoria-Chaparro J. Eritema multiforme. In: Restrepo-Castaño A, Franco RS, editors. Dermatología. Octava edición. Medellín, Colombia: Corporación para Investigaciones Biológicas; 2017. p. 129-37.
Walicka M, Majsterek M, Rakowska A, Słowińska M, Sicińska J, Góralska B, et al. Mycoplasma pneumoniae-induced pneumonia with StevensJohnson syndrome of acute atypical course. Polish Arch Intern Med. 2008;118:449-53. https://doi.org/10.20452/pamw.452
Domínguez-Borgua A, González I, Morales L, Martinez-Carrillo MF, Palacios P. Toxic epidermal necrolysis and development of liver abscesses. Gac Med Mex. 2015;151:512-8.
Uzun R, Yalcin AD, Celik B, Bulut T, Yalcin AN. Levofloxacin induced toxic epidermal necrolysis: Successful therapy with omalizumab (antiIgE) and pulse prednisolone. Am J Case Rep. 2016;17:666-71. https://doi.org/10.12659/AJCR.899823
Yang CY, Dao RL, Lee TJ, Lu CW, Yang CH, Hung SI, et al. Severe cutaneous adverse reactions to antiepileptic drugs in Asians. Neurology. 2011;77:2025-33. https://doi.org/10.1212/WNL.0b013e31823b478c
Godhwani N, Bahna SL. Antiepilepsy drugs and the immune system. Ann Allergy Asthma Immunol. 2016;117:634-40. https://doi.org/10.1016/j.anai.2016.09.443
Harr T, French LE. Toxic epidermal necrolysis and Stevens Johnson syndrome. Orphanet J Rare Dis. 2010;5:1-11. https://doi.org/10.1186/1750-1172-5-39
Changela A, Javaiya H, Rickenback K, Elnawawi A, Changela K. Toxic epidermal necrolyis after vancomycin use: A case report and discussion of management. Am J Ther. 2013;20:223-5. https://doi.org/10.1097/MJT.0b013e3181f94c27
Harris V, Jackson C, Cooper A. Review of toxic epidermal necrolysis. Int J Mol Sci. 2016;17:1-11. https://doi.org/10.3390/ijms17122135
Lim VM, Do A, Berger TG, Nguyen AH, Deweese J, Malone JD, et al. A decade of burn unit experience with Stevens-Johnson syndrome/toxic epidermal necrolysis: Clinical pathological diagnosis and risk factor awareness. Burns. 2016;42:836-43. https://doi.org/10.1016/j.burns.2016.01.014
Brickel N, Shaikh H, Kirkham A, Davies G, Chalker M, Yoshida P. Collaboration in pharmacovigilance: lamotrigine and fatal severe cutaneous adverse reactions - a review of spontaneous reports. Ther Clin Risk Manag. 2017;13:897-903. https://doi.org/10.2147/TCRM.S131021
Dodiuk-Gad RP, Chung WH, Valeyrie-Allanore L, Shear NH. Stevens-Johnson syndrome and toxic epidermal necrolysis: An update. Am J Clin Dermatol. 2015;16:475-93. https://doi.org/10.1007/s40257-015-0158-0
Galindo-Díaz LF, Díaz-Guío DA. Insuficiencia cutánea aguda. En: Díaz-Guío DA, editor. Cuarta edición. Armenia, Quindío: Publicaciones Vital Care Cuidado Crítico; 2013. p. 478-86.
Paradisi A, Abeni D, Bergamo F, Ricci F, Didona D, Didona B. Etanercept therapy for toxic epidermal necrolysis. J Am Acad Dermatol. 2014;71:278-83. https://doi.org/10.1016/j.jaad.2014.04.044
Yang LP, Zhang AL, Wang DD, Ke HX, Cheng Q, Wang C. Stevens-Johnson syndrome induced by the cross-reactivity between teicoplanin and vancomycin. J Clin Pharm Ther. 2014;39:442-5. https://doi.org/10.1111/jcpt.12159
Arshad F, Bhat TS, Lone AR. Docetaxel induced Lyell's syndrome: A rare life threatening cause of dermatitis medicamentosas. J Cancer Res Ther. 2014;10:742-4.
Creamer D, Walsh SA, Dziewulski P, Exton LS, Lee HY, Dart JKG, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. J Plast Reconstr Aesthetic Surg. 2016;69:e119-227. https://doi.org/10.1016/j.bjps.2016.01.034
Yamane Y, Matsukura S, Watanabe Y, Yamaguchi Y, Nakamura K, Kambara T, et al. Retrospective analysis of Stevens-Johnson syndrome and toxic epidermal necrolysis in 87 Japanese patients - Treatment and outcome. Allergol Int. 2016;65:74-81. https://doi.org/10.1016/j.alit.2015.09.001
De Prost N, Mekontso-Dessap A, Valeyrie-Allanore L, van Nhieu JT, Duong TA, Chosidow O, et al. Acute respiratory failure in patients with toxic epidermal necrolysis: Clinical features and factors associated with mechanical ventilation. Crit Care Med. 2014;42:118-28. https://doi.org/10.1097/CCM.0b013e31829eb94f
Bastuji-Garin S, Fouchard N, Bertocchi M, Roujeau JC, Revuz J, Wolkenstein P. Scorten: A severity-ofillness score for toxic epidermal necrolysis. J Invest Dermatol. 2000;115:149-53. https://doi.org/10.1046/j.1523-1747.2000.00061.x
Seczynska B, Nowak I, Sega A, Kozka M, Wodkowski M, Szczeklik W. Supportive therapy for a patient with toxic epidermal necrolysis undergoing plasmapheresis. Crit Care Nurse. 2013;33:26-38. https://doi.org/10.4037/ccn2013555
Schneider JA, Cohen PR. Stevens-Johnson syndrome and toxic epidermal necrolysis: A concise review with a comprehensive summary of therapeutic interventions emphasizing supportive measures. Adv Ther. 2017;34:1235-44. https://doi.org/10.1007/s12325-017-0530-y
World Health Organization. WHO's cancer pain ladder for adults [Internet]; 2013. Fecha de consulta: 18 de febrero de 2018. Disponible en: http://www.who.int/cancer/palliative/painladder/en/.
Sekula P, Dunant A, Mockenhaupt M, Naldi L, Bouwes Bavinck JN, Halevy S, et al. Comprehensive survival analysis of a cohort of patients with Stevens-Johnson syndrome and toxic epidermal necrolysis. J Invest Dermatol. 2013;133:1197204. https://doi.org/10.1038/jid.2012.510
Wolf R, Davidovici B. Severe cutaneous adverse drug reactions: Who should treat, where and how? Facts and controversies. Clin Dermatol. 2010;28:344-8. https://doi.org/10.1016/j.clindermatol.2009.06.020
Paquet P, Piérard GE. New insights in toxic epidermal necrolysis ( Lyell' syndrome). Drug Saf. 2010;33:189-212. https://doi.org/10.2165/11532540-000000000-00000
Saavedra C, Cárdenas P, Castellanos H, Contreras K, Castro JR. Cephazolin-induced toxic epidermal necrolysis treated with intravenous immunoglobulin and N-acetylcysteine. Case Reports Immunol. 2012;2012:1-4. https://doi.org/10.1155/2012/931528
Husain Z, Reddy BY, Schwartz RA. DRESS syndrome: Part I. Clinical perspectives. J Am Acad Dermatol. 2013;68:693.e1-693.e14. https://doi.org/10.1016/j.jaad.2013.01.033
Shiohara T, Kano Y. Drug reaction with eosinophilia and systemic symptoms (DRESS): Incidence, pathogenesis and management. Expert Opin Drug Saf. 2017;16:139-47.
EL omairi N, Abourazzak S, Chaouki S, Atmani S, Hida M. Drug reaction with eosinophilia and systemic symptom (DRESS) induced by carbamazepine: Case report and literature review. PanAfrican Med J. 2014;8688:1-4. https://doi.org/10.11604/pamj.2014.18.9.3799
Kimmoun A, Dubois E, Perez P, Barbaud A, Levy B. Shock state: An unrecognized and underestimated presentation of drug reaction with eosinophilia and systemic symptoms. Shock. 2013;40:387-91. https://doi.org/10.1097/SHK.0000000000000041
Chen YC, Cho YT, Chang CY, Chu CY. Drug reaction with eosinophilia and systemic symptoms: A drug-induced hypersensitivity syndrome with variable clinical features. Dermatologica Sin. 2013;31:196-204. https://doi.org/10.1016/j.dsi.2013.09.006
Błaszczyk B, Lasoń W, Czuczwar SJ. Antiepileptic drugs and adverse skin reactions: An update. Pharmacol Reports. 2015;67:426-34. https://doi.org/10.1016/j.pharep.2014.11.009
Sasidharanpillai S, Riyaz N, Rajan U, Binitha M, Khader A, Reena Mariyath O, et al. Drug reaction with eosinophilia and systemic symptoms: Observations from a tertiary care institution. Indian J Dermatol Venereol Leprol. 2014;80:221-8. https://doi.org/10.4103/0378-6323.132249
Ichai P, Laurent-Bellue A, Saliba F, Moreau D, Besch C, Francoz C, et al. Acute liver failure/injury related to drug reaction with eosinophilia and systemic symptoms: Outcomes and prognostic factors. Transplantation. 2017;101:1830-7. https://doi.org/10.1097/TP.0000000000001655
Hamm RL. Drug-hypersensitivity syndrome: Diagnosis and treatment. J Am Coll Clin Wound Spec. 2011;3:77-81. https://doi.org/10.1016/j.jcws.2012.06.001
Spriet S, Banks TA. Drug reaction with eosinophilia and systemic symptoms syndrome. Allergy Asthma Proc. 2015;36:501-5. https://doi.org/10.2500/aap.2015.36.3903
Miyazu D, Kodama N, Yamashita D, Tanaka H, Inoue S, Imakyure O, et al. DRESS syndrome caused by cross-reactivity between vancomycin and subsequent teicoplanin administration: A case report. Am J Case Rep. 2016;17:625-31. https://doi.org/10.12659/AJCR.899149
Nam YH, Park MR, Nam HJ, Lee SK, Kim KH, Roh MS, et al. Drug reaction with eosinophilia and systemic symptoms syndrome is not uncommon and shows better clinical outcome than generally recognised. Allergol Immunopathol (Madr). 2015;43:19-24. https://doi.org/10.1016/j.aller.2013.08.003
Moriceau F, Prothet J, Blaise BJ, Ben Said B, Page M, Ber CE, et al. DRESS syndrome in the ICU: When a patient Is treated with multiple drugs. Case Reports Crit Care. 2016;2016:1-4. https://doi.org/10.1155/2016/9453286
Criado PR, Criado RFJ, Avancini J de M, Santi CG. A case of drug reaction with eosinophilia and systemic symptoms. An Bras Dermatol. 2012;87:435-49. https://doi.org/10.1590/S0365-05962012000300013
Borok J, Hau J, Worswick S. Adult with morbilliform rash and tattoo bullae. Dermatol Online J. 2016;22:3-7.
Thongsri T, Chularojanamontri L, Pichler W j. Cardiac involvement in DRESS syndrome. Asian Pacific J Allergy Immunol. 2017;35:3-10.
Husain Z, Reddy BY, Schwartz RA. DRESS syndrome: Part II. Management and therapeutics. J Am Acad Dermatol. 2013;68:709.e1-709.e9. https://doi.org/10.1016/j.jaad.2013.01.032
Ocampo-Garza J, Ocampo-Garza SS, MartínezVillarreal JD, Barbosa-Moreno LE, Guerrero-González GA, Ocampo-Candiani J. Reacción por drogas con eosinofilia y síntomas sistémicos (síndrome de DRESS). Estudio retrospectivo de nueve casos. Rev Med Chil. 2015;143:577-83. https://doi.org/10.4067/S0034-98872015000500004
Cómo citar
Descargas
Descargas
Publicado
Cómo citar
Número
Sección
Licencia

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-CompartirIgual 4.0.
| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |