Langerhans cell histiocytosis. Ten-year experience in The National Institute of Cancer of Colombia
Keywords:
Langerhans cell histiocytosis, skin manifestationsAbstract
Introducción: Langerhans cell histiocytosis (LCH) is a rare proliferative disorder of histiocytes characterized by a proliferation of abnormal and clonal Langerhans cells. The disease presents varied clinical manifestations. Descriptions of Hispanic patients have been scarce.
Methods: Clinical profile, disease-distribution and outcome of 34 cases of LCH from January 1988 to December 1999 is presented in this retrospective analysis based on the hospital records, with special interest in skin disorders.
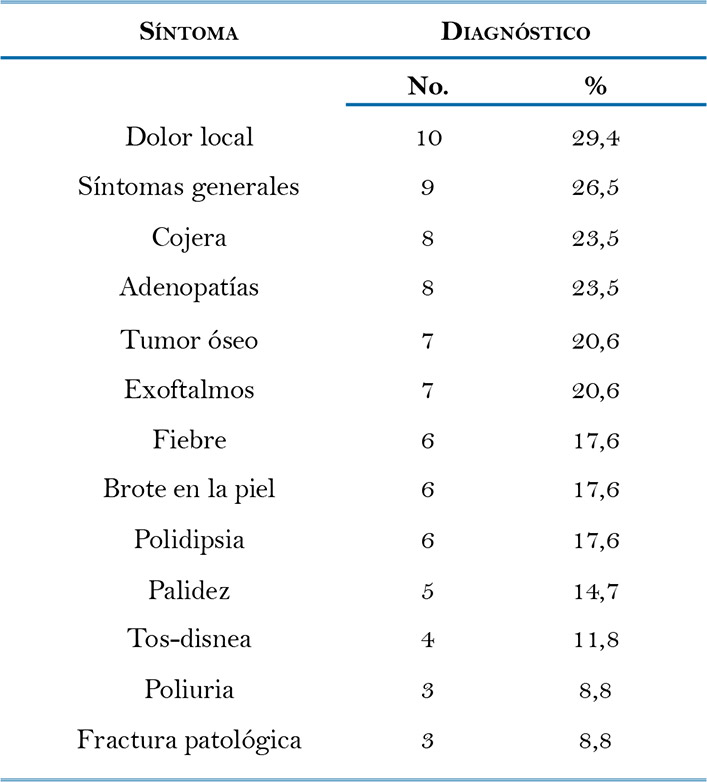
Results: The age ranged from 4 months to 47 years, median age 3 years. Multisystem disease was documented in 16 (47%) patients. The most common type of skin lesion was papular rash in 8 (23.5%) patients. During a mean time follow-up period of 3.48 years, 7 (20.5%) patients died. Cases with localized or cutaneous limited disease received topical steroids, radiotherapy, cryosurgery, and oral steroids while most of cases with disseminated/multi-system disease were treated with prednisolone and, vinblastine or etoposide.
Conclusion: General outcome of the LCH in the National Cancer Institute of Colombia is similar to that described in other large series of patients.
Author Biographies
Santiago Andrés Ariza
Especialista en Dermatología. Fellow en Dermatología Oncológica. Instituto Nacional de Cancerología, Bogotá.
Andrés Felipe Cardona
Especialista en Epidemiología, Universidad del Rosario. Especialista en Medicina Interna. Especialista en Oncología Clínica. Instituto Nacional de Cancerología. Bogotá.
Xavier Rueda
Especialista en Dermatología Oncológica. Servicio de Dermatología Oncológica. Instituto Nacional de Cancerología. Bogotá.
References
2. William CL, Busque L, Griffith BB, McClain KL, Duncan MH, Gilliland DG. Langerhans cell histiocytosis (histiocytosis X) – a clonal proliferative disease. N Engl J Med 1994; 331:154-60.
3. Caputo R. Langerhans cell histiocytosis. Fistzpatrick TB, Freedber IM, Eisen A, Austen KF, Goldsmith LA, Katz SI, editors. In: Dermatology in General Medicine, ed 5. New York, Mc Graw-Hill. 1998. Vol 2; .p. 1882 – 92.
4. Yu RC, Chu C, Buluwela L, Chu AC. Clonal proliferation of Langerhans cells in Langerhans cell histiocytosis. Lancet 1994; 343: 767-8.
5. The French Langerhans Cell Histiocytosis Study Group. A multicentre retrospective survey of Langerhans cell histiocytosis: 348 cases observed between 1983 and 1993. Arch Dis Child 1996;75:17-24.
6. Kilpatrick S, Wenger D, Gilchris G, Shives T, Wollan P. Langerhans cell histiocytosis (Histiocytosis X) of Bone. Cancer 1995;76: 2471-84.
7. Howarth DM, Gilchrist GS, Mullan BP, Wiseman GA, Edmonson JH, Schomberg PJ. Langerhans cell histiocytosis. Diagnosis, natural history, management, and outcome. Cancer 1999; 85: 2278-90.
8. Willis B, Ablin A, Weinberg V, Zoger S, Wara WM, Matthay KK. Disease course and late sequelae of Langerhans cell histiocytosis: 25-year experience at the University of California, San Francisco. J Clin Oncol 1996;14: 2073.
9. Belaich S. Langerhans cell histiocytosis. Dermatology 1994; 189(supl 2): 2-7.
10. Stockschlaeder M, Sucker C. Adult Langerhans cell histiocytosis. Eur J Haematol 2006; 76: 363–8.
11. Sundar KM, Gosselin MV, Chung HL, Cahill BC. Chest 2003; 123:1673-83.
12. Nezelof C, Basset F. An hypothesis of Langerhans cell histiocytosis: the failure of the immune system to switch from an innate to an adaptive mode. Pediatr Blood Cancer 2004; 42: 398–400.
13. Savasan S. An enigmatic disease: childhood Langerhans cell histiocytosis in 2005. International Journal of Dermatology 2006; 45: 182–8.
14. Egeler RM, Neglia JP, Aricò M, Favara BE, Heitger A, Nesbit ME. Acute leukemia in association with Langerhans cell histiocytosis. Med Pediatr Oncol 1994; 23: 81–5.
15. Egeler RM, Neglia JP, Puccetti DM, Brennan CA, Nesbit ME. Association of Langerhans cell histiocytosis with malignant neoplasms. Cancer 1993; 71: 865–73.
16. Wolfson S, Botero F, Hurwitz S, Pearson H. Pure cutaneous histicytosis X. Cancer 1981; 48: 2236-8.
17. Aricó M, Egeler RM. Clinical aspects of Langerhans cell histiocytosis. Hematol Oncol Clin N Am 1998; 12:247-57.
How to Cite
Downloads
Downloads
Published
How to Cite
Issue
Section
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |






