Cutaneous manifestations of fulminant sepsis by Staphylococcus aureus: An autopsy study.
Keywords:
Staphylococcus aures, skin, autopsy, septic shockAbstract
Introduction: Systemic infections by S. aureus are an important cause of hospital morbidity and mortality. Adequate clinical assessment of cutaneous manifestations could allow an opportune diagnosis of S. aureus septicemia.
Objective: To describe the cutaneous manifestations on deaths caused by S. aureus septic shock.
Materials and Methods: Prospective descriptive study of autopsy cases..
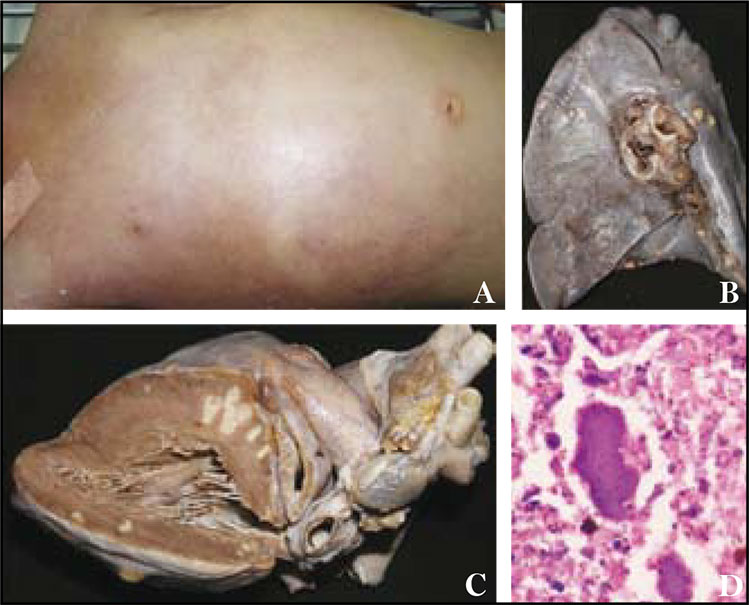
Results: Nine autopsies of patients with a clinical cause of death of S. aureus septic shock were analyzed. The cases represent the 3.1% of the total autopsies performed by the institution during that year (9/285). Mean age of the cases was 15.8 years (range, 2 to 47), seven males and two females (male/female relationship, 3.5:1). All patients adquired the infection in the community. The clinical manifestations evolved during four to six days. However, only in three cases an appropriate clinical diagnosis was made. Microbiological diagnosis of S. aureus was documented in all cases. The primary focus was the skin in seven patients and the osteoarticular system in two patients. Cutaneous macroscopic alterations included generalized pustules (5 cases), generalized petechial erythema with subcutaneous edema (2 cases), and a vesicular-pustulous varicelliform eruption (2 cases). Histologically, a septic vasculitis were found in the seven patients with generalized pustules. In the cases of generalized erythema the biopsies showed mononuclear perivascular superficial infiltrate and edema.
Conclusions: Septic shock by S. aureus is associated with multiple cutaneous manifestations which allows the identification of the disease.
Author Biographies
Julio Cesar Mantilla
Patólogo y Antropólogo Forense. Jefe del Departamento de Patología de la Universidad Industrial de Santander. Grupo de Investigación en Patología Tropical, Infecciosa y Extraordinaria. Universidad Industrial de Santander, Bucaramanga, Colombia.
Armando José Vásquez
Dermatólogo. Asesor clínico del Departamento de Patología de la Universidad Industrial de Santander. Grupo de Investigación en Patología Tropical, Infecciosa y Extraordinaria. Universidad Industrial de Santander, Bucaramanga, Colombia
Julio Alexander Díaz
Residente de tercer año en Patología. Especialista en metodología de la investigación. Grupo de Investigación en Patología Tropical, Infecciosa y Extraordinaria. Universidad Industrial de Santander, Bucaramanga, Colombia.
References
2. Prescott ML, Harley JP y Klein DA. Microbiología, 4a. Ed. McGraw-Hill Interamericana 1999; pag 713 y 812.
3. Landaeta JM. Estafilococos coagulasa-negativos: una aproximación microbiológica. Bol Soc Ven Micr. 1998; 18: 71-8.
4. Lowy FD. Staphylococcus aureus Infections. J Engl J Med. 1998; 339: 520-32.
5. Sheagren JN. Staphylococcus aureus: the persistent pathogen. N Engl J Med 1984; 310:1368-73, 1437.
6. Santamaría V, Alvarado A. Flora cutánea como protección y barrera de la piel normal. Rev Cent Dermatol Pascua. 2002; 11:18-210.
7. Marrack P, Kappler J. The staphylococcal enterotoxins and their relatives. Science 1990; 248:705-711. [Erratum, Science 1990;248:1066.]
8. Harris TO, Grossman D, Kappler JW, Marrack P, Rich RR, Betley MJ. Lack of complete correlation between T-cellstimulatory activities of staphylococcal enterotoxins. Infect Immun 1993; 61: 3175 - 83.
9. Herold BC, Immergluck LC, Maranan MC, Lauderdale DS, Gaskin RE, Boyle-Vavra S, Leitch CD, Daum RS. Communityacquired methicillin-resistant Staphylococcus aureus in children with no identified predisposing risk. JAMA. 1998;279:593-8.
10. Wenzel RP, Perl TM. The significance of nasal carriage of Staphylococcus aureus and the incidence of postoperative wound infection. J Hosp Infect. 1995; 31:13-24.
11. Tuazon CU, Perez A, Kishaba T, Sheagren JN. Staphylococcus aureus among insulin-injecting diabetic patients: an increased carrier rate. JAMA. 1975; 231:1272.
12. Tuazon CU, Sheagren JN. Increased rate of carriage of Staphylococcus aureus among narcotic addicts. J Infect Dis. 1974; 129:725-7.
13. Yu VL, Goetz A, Wagener M, Smith PB, Rihs JD, Hanchett J, Zuravleff JJ. Staphylococcus aureus nasal carriage and infection in patients on hemodialysis: efficacy of antibiotic prophylaxis. N Engl J Med. 1986; 315: 91-6.
14. Weinke T, Schiller R, Fehrenbach FJ, Pohle HD. Association between Staphylococcus aureus nasopharyngeal colonization and septicemia in patients infected with the human immunodeficiency virus. Eur J Clin Microbiol Infect Dis 1992;11:985-9.
15. Speller DCE, Johnson AP, James D, Marples RR, Charlett A, George RC. Resistance to methicillin and other antibiotics in isolates of Staphylococcus aureus from blood and cerebrospinal fluid, England and Wales, 1989-95. Lancet 1997; 350:323-325 Pediatrics 2005; 115: 642-8.
16. González BE, Martínez-Aguilar G, Hulten KG, Hammerman, WA, Coss-Bu J, Avalos-Mishaan A, Mason EO Jr, Kaplan L. Severe Staphylococcal Sepsis in Adolescents in the Era of Community-Acquired Methicillin-Resistant Staphylococcus aureus. Pediatrics 2005; 115: 642-8.
17. Martin TC, Stranahan P, Rivero JC. A fatal case of community acquired methicillin resistant Staphylococcus aureus brain abscess in a previously healthy adolescent. West Indian Med J. 2006; 55: 200-4.
18. Kim HS, Weilbaecher DG, Lie JT, Titus JL. Myocardial abscesses. Am J Clin Pathol. 1978; 70:18-23.
19. Ansaloni L. Tropical pyomyositis. World J Surg. 1996; 20:613–7.
20. Donatto K. Orthopedic management of septic arthritis. Rheumatic Disease Clinics of North America. 1998; 24: 275 - 86.
How to Cite
Downloads
Downloads
Published
How to Cite
Issue
Section
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |






