CHROMOMYCOSIS, A FORGOTTEN TROPICAL DISEASE: A CASE REPORT AND REVIEW OF THE LITERATURE
DOI:
https://doi.org/10.29176/2590843X.1590Keywords:
Chromoblastomycosis, Chromomycosis, Dematiaceous fungi, Subcutaneous mycosesAbstract
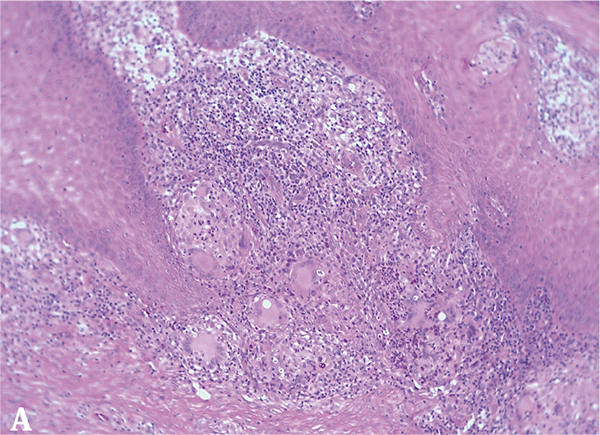
Introduction: Chromomycosis is a chronic, progressive and granulomatous fungal infection with different manifestations in the skin and subcutaneous cellular tissue. It caused by multiple species of as dematiaceous fungi. The infection manifests as plaques of slow growth, exophytic, desquamative with black spots on its surface. The diagnosis is made with the clinical manifestations and demonstration of the fungus.
Methodology: It is a clinical case report and narrative review of the literature between the period 2000 - 2021, in the PubMed and Scopus databases, using the keywords Chromomycosis, Chromoblastomycosis,
Chromoblastomycoses, Dermatitis Verrucosa, Chromomycoses, Dematiaceous fungi and Subcutaneous mycoses.
Results: We present the case of a 54-year-old man with a diagnosis of long-standing chromomycosis from a rural area in the department of Meta, Colombia. The epidemiology, etiology, pathogenesis, clinical manifestations, complications, diagnosis, therapeutic principles, follow-up and prognosis of this pathology are discussed.
Conclusions: Chromomycosis is a fungal infection usually found in tropical and subtropical areas, however, publications in recent years have changed the epidemiological perspective, It is currently considered a cosmopolitan infection, with reported cases on five continents. The clinical concepts have been maintained over time; New diagnostic methods have been proposed which are not widely available and It remains a real
therapeutic challenge as cure rates are not high and It´s often refractory to different managements.
Author Biographies
Heliana Marcela Botello-Mojica, Médica residente de tercer año de Dermatología. Semillero de Investigación en Dermatología (SIDERM). Universidad de Caldas, departamento clínico, Manizales, Colombia.
Médica residente de tercer año de Dermatología. Semillero de Investigación en Dermatología (SIDERM). Universidad de Caldas, departamento clínico, Manizales, Colombia.
Lucía Vanden en den-Medina, Médica dermatóloga. Docente de Dermatología. Semillero de Investigación en Dermatología (SIDERM). Universidad de Caldas, departamento clínico, Manizales, Colombia.
Médica dermatóloga. Docente de Dermatología. Semillero de Investigación en Dermatología (SIDERM). Universidad de Caldas, departamento clínico, Manizales, Colombia.
Felipe Jaramillo- Ayerbe, Médico dermatólogo. Dermatopatólogo. Docente de Dermatología. Semillero de Investigación en Dermatología (SIDERM). Universidad de Caldas, departamento clínico, Manizales, Colombia.
Médico dermatólogo. Dermatopatólogo. Docente de Dermatología. Semillero de Investigación en Dermatología (SIDERM). Universidad de Caldas, departamento clínico, Manizales, Colombia.
Mayra Alejandra Marulanda-Galvis, Estudiante de internado de Medicina. Semillero de Investigación en Dermatología (SIDERM). Universidad de Caldas, departamento clínico, Manizales, Colombia.
Estudiante de internado de Medicina. Semillero de Investigación en Dermatología (SIDERM). Universidad de Caldas, departamento clínico, Manizales, Colombia.
References
de Brito AC, Semblano MJS. Chromoblastomycosis: an etiological, epidemiological, clinical, diagnostic, and treatment update. An Bras Dermatol [Internet]. 2018;93(4):495-506. http://dx.doi.org/10.1590/abd1806-4841.20187321
Santos ALS, Palmeira VF, Rozental S, Kneipp LF, Nimrichter L, Alviano DS, Rodrigues ML, Alviano C. Biology and pathogenesis of Fonsecaea pedrosoi, the major etiologic agent of chromoblastomycosis. FEMS Microbiol Rev [Internet]. 2007;31(5):570-91. http://dx.doi.org/10.1111/j.1574-6976.2007.00077.x
Torres-Guerrero E, Isa-Isa R, Isa M. Chromoblastomycosis. Clin Dermatol [Internet]. 2012;30(4):403-8. http://dx.doi.org/10.1016/j.clindermatol.2011.09.011
Bonifaz A, Carrasco-Gerard E, Saul A. Chromoblastomycosis: clinical and mycologic experience of 51 cases. Mycoses [Internet]. 2001;44(1-2):1-7. http://dx.doi.org/10.1046/j.1439-0507.2001.00613.x
Queiroz-Telles F, de Hoog S, Santos DWCL, Salgado CG, Vicente VA, Bonifaz A, et al. Chromoblastomycosis. Clin Microbiol Rev [Internet]. 2017;30(1):233-76. http://dx.doi.org/10.1128/CMR.00032-16
Burstein Z. Cromomicosis: Clínica y Tratamiento; situación epidemiológica en Latinoamérica. Med Exp [Internet]. 2004;21(3):167-75. Disponible en: https://bit.ly/2OzDUHA
Queiróz AJR, Pereira Domingos F, Antônio JR. Chromoblastomycosis: clinical experience and review of literature. Int J Dermatol [Internet]. 2018;57(11):1351-5. http://dx.doi.org/10.1111/ijd.14185
de Andrade TS, de Almeida AMZ, Basano S de A, Takagi EH, Szeszs MW, Melhem MSC, et al. Chromoblastomycosis in the Amazon region, Brazil, caused by Fonsecaea pedrosoi, Fonsecaea nubica, and Rhinocladiella similis: Clinicopathology, susceptibility, and molecular identification. Med Mycol. 2020;58(2):172-80. http://dx.doi.org/10.1093/mmy/myz034
Filho RVT. Chromoblastomycosis: A neglected disease. 2019;65(9):1130-2. http://dx.doi.org/10.1590/1806-9282.65.9.1130
Queiroz-Telles F, McGinnis MR, Salkin I, Graybill JR. Subcutaneous mycoses. Infect Dis Clin North Am [Internet]. 2003;17(1):59-85. http://dx.doi.org/10.1016/S0891-5520(02)00066-1
Tyring S, Lupi O, Hengge U. Subcutaneous Mycoses. En: Tropical Dermatology [Internet]. 2.a edición. Elsevier; 2017. p. 202-18. Disponible en: https://bit.ly/3v9rwyG
Ameen M. Chromoblastomycosis: clinical presentation and management. Clin Exp Dermatol [Internet]. 2009;34(8):849-54. http://dx.doi.org/10.1111/j.1365-2230.2009.03415.x
Gaviria-Giraldo CM C-CN. Esporotricosis y cromoblastomicosis: revisión de la literatura. CES Med [Internet]. 2017;31(1):77-91. http://dx.doi.org/10.21615/
Qiu Y, Zhang J, Tang Y, Zhong X, Deng J. Case report: Fever- pneumonia- lymphadenectasis- osteolytic-subcutaneous nodule: Disseminated chromoblastomycosis caused by phialophora. J Infect Chemother. 2019;25(12):1031-6. http://dx.doi.org/10.1016/j.jiac.2019.05.002
De Azevedo CMPS, Gomes RR, Vicente VA, Santos DWCL, Marques SG, Do Nascimento MMF, et al. Fonsecaea pugnacius, a novel agent of disseminated chromoblastomycosis. J Clin Microbiol. 2015;53(8):2674-85. http://dx.doi.org/10.1128/JCM.00637-15
Marques SG, Bomfim MRQ, Azevedo C de MPS, Martins CVB, Marques ACG, Gonçalves AG, et al. Mixed secondary bacterial infection is associated with severe lesions of chromoblastomycosis in a neglected population from Brazil. Diagn Microbiol Infect Dis. 2019;95(2):201-7. http://dx.doi.org/10.1016/j.diagmicrobio.2019.05.018
Schneider GX, Gomes RR, Bombassaro A, Zamarchi K, Voidaleski MF, Costa FF, et al. New Molecular Markers Distinguishing Fonsecaea Agents of Chromoblastomycosis. Mycopathologia. 2019;184(4):493-504. http://dx.doi.org/10.1007/s11046-019-00359-2
Belda W, Criado PR, Passero LFD. Successful treatment of chromoblastomycosis caused by Fonsecaea pedrosoi using imiquimod. J Dermatol. 2020;47(4):409-12. http://dx.doi.org/10.1111/1346-8138.15225
Belda W, Criado PR, Domingues Passero LF. Case Report: Treatment of Chromoblastomycosis with Combinations including Acitretin: A Report of Two Cases. Am J Trop Med Hyg. 2020;103(5):1852-4. http://dx.doi.org/10.4269/ajtmh.20-0471
Sendrasoa FA, Rakotoarisaona MF, Ranaivo IM, Razanakoto NH, Sata M, Raharolahy O, et al. [Management of chromoblastomycosis, a challenge for limited-resource countries such as Madagascar]. Ann Dermatol Venereol. 2020;147(5):377-82. http://dx.doi.org/10.1016/j.annder.2020.01.018
How to Cite
Downloads
Downloads
Published
How to Cite
Issue
Section

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |






