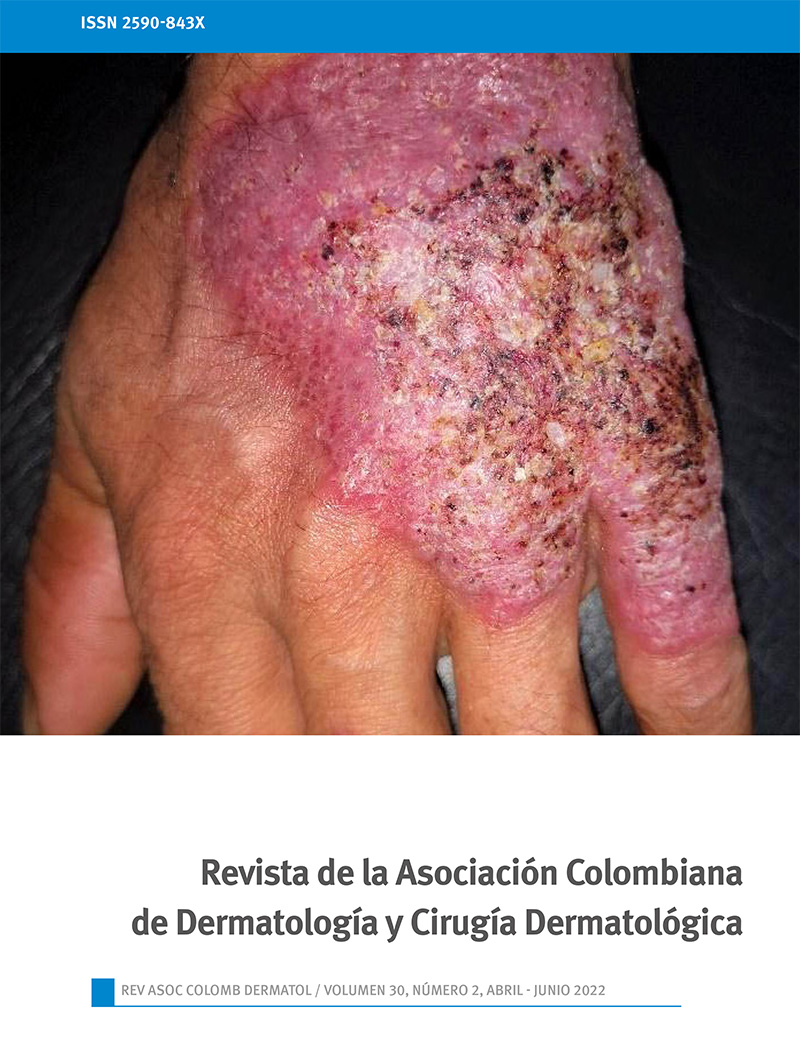
Lobomycosis in a military soldier from Chocó
DOI:
https://doi.org/10.29176/2590843X.1675Keywords:
Keloid; Lacazia loboi; Lobomycosis; Subcutaneous mycosisAbstract
Lobomycosis is a rare subcutaneous mycosis, prevalent in the tropical and subtropical regions of Central and South America, with a predominance in the Amazon forest. It is caused by the traumatic implantation of the Lacazia loboi fungus in the skin and subcutaneous tissue. Its clinical manifestations are solitary or multiple keloid-type dermal nodules that converge to form slow-growing, painless plaques. Diagnosis is
made by histopathological identification of the fungus. For treatment, surgical removal of the lesions is the choice, associated with itraconazole and clofazimine when there are disseminated lesions, but the results are not highly effective as reported in the literature. We present a case of Lobomycosis in a male professional soldier of the National Army from Choco, who initially presented a papule with subsequent progression to a nodule on the left leg of 15 years of evolution. In this article we highlight the clinical and diagnostic characteristics of the diseas
References
Carrasco-Zuber JE, Navarrete-Dechent C, Bonifaz A, Fich F, Vial-Letelier V, Berroeta-Mauriziano D. Cutaneous Involvement in the Deep Mycoses: A Literature Review. Part I-Subcutaneous Mycoses. Actas Dermosifiliogr. 2016 Dec;107(10):806-815. English, Spanish. doi: https://doi.org/10.1016/j.ad.2016.05.017
Carvalho KA, Floriano MC, Enokihara MM, Mascarenhas MR. Jorge Lobo's disease. An Bras Dermatol. 2015 Jul-Aug;90(4):586-8. doi: https://doi.org/10.1590/abd1806-4841.20153603
Goihman-Yahr M. Update on Jorge Lobo's disease. Int J Dermatol. 2008 Jun;47(6):630. doi: https://doi.org/10.1111/j.1365-4632.2008.03560.x.
Reif JS, Schaefer AM, Bossart GD. Lobomycosis: risk of zoonotic transmission from dolphins to humans. Vector Borne Zoonotic Dis. 2013 Oct;13(10):689-93. doi: https://doi.org/10.1089/vbz.2012.1280.
Arenas CM, Rodriguez-Toro G, Ortiz-Florez A, Serrato I. Lobomycosis in Soldiers, Colombia. Emerg Infect Dis. 2019 Apr;25(4):654-660. doi: https://doi.org/10.3201/eid2504.181403
Bolognia JL, Jorizzo JL, Rapini RP.Dermatology Book, 2012, 3rd Ed. Elsevier.
Talhari S, Talhari C. Lobomycosis. Clin Dermatol. 2012 Jul-Aug;30(4):420-4. doi: https://doi.org/10.1016/j.clindermatol.2011.09.014.
Fonseca JJ. Lobomycosis. Int J Surg Pathol. 2007 Jan;15(1):62-3. doi: https://doi.org/10.1177/1066896906295684
Claudia A, Lorena S, John B y Gerzain R. Síndrome verrucoso tropical. Piel (BARC). 2016. Elsevier, España. https://doi.org/10.1016/j.piel.2016.02.011
Araújo MG, Cirilo NS, Santos SNMBD, Aguilar CR, Guedes ACM. Lobomycosis: a therapeutic challenge. An Bras Dermatol. 2018 Mar;93(2):279-281. doi: https://doi.org/10.1590/abd1806-4841.20187044.
How to Cite
Downloads
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Revista de la Asociación Colombiana de Dermatología y Cirugía Dermatológica

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |