Stevens Johnson syndrome and toxic epidermal necrolysis at the Hospital Universitario del Valle “Evaristo García” for a period of 9 years.
DOI:
https://doi.org/10.29176/2590843X.256Keywords:
Stevens Johnson, syndrome, toxic epidermal necrolysis, tumor necrosis factor alpha, pentoxifyllineAbstract
The Stevens-Johnson syndrome and the toxic epidermal necrolysis are very severe cutaneous drug reactions and constitute a spectrum of the same disease, sharing etiological, pathogenic, histological and therapeutic aspects.
Objectives: To describe the cases of toxic epidermal necrolysis and Stevens-Johnson syndrome over a nine year period at the Hospital Universitario del Valle, the treatments used in these patients and their mortality.
Methodology: A medical history review was carried out retrospectively of patients with Stevens-Johnson syndrome and toxic epidermal necrolysis diagnosed and managed from February, 2003, until April, 2012, at the Hospital Universitario del Valle. We analyzed clinical characteristics, frequency, mortality, medications as possible triggers, treatments used and response to them.
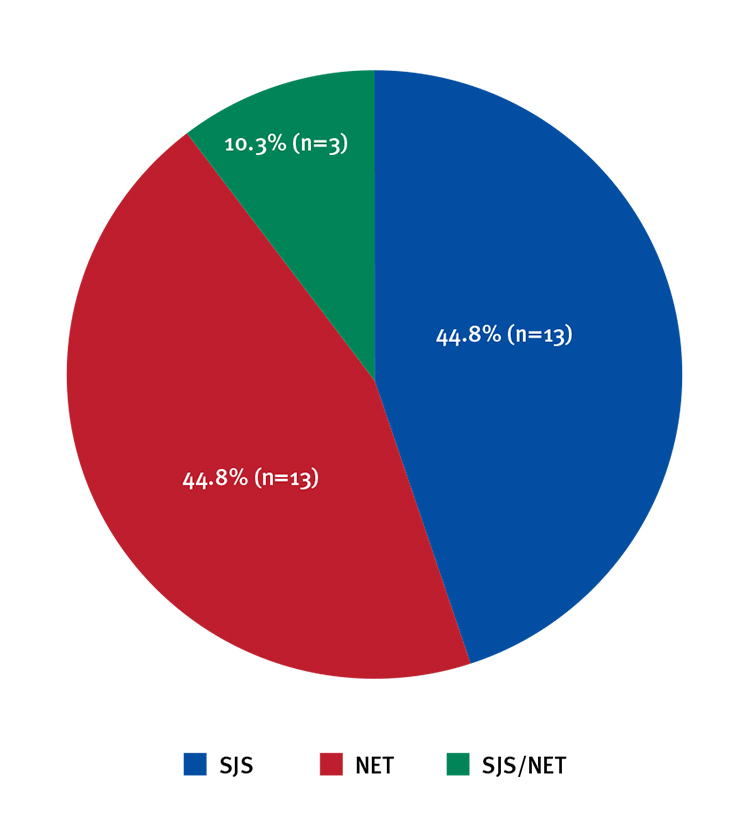
Results: Out of 29 cases, 13 (44.8%) had diagnosis of toxic epidermal necrolysis, 13 (44.8%) had Stevens-Johnson syndrome and the remaining 3 (10.3%), overlapping Stevens-Johnson syndrome-toxic epidermal necrolysis. In 16 patients (55%) a single drug could be the trigger. In 12 patients (41%) two or more drugs were found as possible triggers. Drugs were identified only in one. Antibiotics, anticonvulsants, NSAIDs and allopurinol were the most frequently associated drugs. All patients received supporting measures. Twenty patients (68%) received antibiotic therapy due to an associated infection. Twenty three patients (79.3%) received pentoxifylline as part of their treatment; six (20.6%) received gammaglobulin (two of them associated with oral pentoxifylline). One patient died (3.4%).
Conclusions: The supporting measures are essential in the management of patients with toxic epidermal necrolysis and Stevens- Johnson syndrome independent of the affected body area, as well as the timely management of complications as superinfection. Pentoxifylline may be considered an alternative in the treatment of these pathologies.
Author Biographies
David Andrés Arias
Médico, residente de Dermatología y Cirugía Dermatológica, Universidad del Valle, Cali, Colombia.
Paola Andrea Londoño
Médica dermatóloga, Universidad del Valle, Cali, Colombia.
Juana Gabriela López
Médica dermatóloga, Universidad del Valle, Cali, Colombia.
Luis Hernando Moreno
Médico dermatólogo, M.Sc. en Microbiología; jefe, Departamento de Dermatología y Cirugía Dermatológica, Universidad del Valle, Cali, Colombia
References
2. García I, Roujeau JC, Cruces M. Necrólisis epidérmica tóxica y síndrome de Stevens-Johnson: clasificación y actualidad terapéutica. Actas Dermosifiliogr. 2000;91:541-51.
3. Criton S, Devi K, Sridevi RK, Asokan RU. Toxic epidermal necrolysis: A retrospective study. Int J Dermatol. 1997;36:923-5.
4. Knowles S, Sheir N. Clinical risk management of Stevens-Johnson syndrome/toxic epidermal necrolysis spectrum. Dermatol Ther. 2009;22:441-51.
5. Jean-AanKoh M, KwangTay Y. An update on Stevens-Johnson syndrome and toxic epidermal necrolysis in children. Curr Opin Pediatr. 2009;21:505-10.
6. 6. Akosa AB, Elhag AM. Toxic epidermal necrolysis. A study of the sweat glands. J Clin Pathol. 1995;22:359-64.
7. Ioannides D, Vakali G, Chrysomallis F, Chaidemenos G, Mpatsios K, Mourellou O, et al. Toxic epidermal necrolysis: A study of 22 cases. J Eur Acad Dermatol Venereol. 1994;3:266-75.
8. Weightman W. Toxic epidermal necrolysis. Australas J Dermatol. 1996;37;167-77.
9. Gerdts B, Vloemans AFPM, Kreis RW. Toxic epidermal necrolysis; 15 years experience in a Dutch burns centre. J Eur Acad Dermatol Venereol. 2007;21:781-8.
10. Chave TA, Mortimer NJ, Sladden MJ, Hall AP, Hutchinson PE. Toxic epidermal necrolysis: Current evidence, practical management and future directions. Br J Dermatol. 2005;153:241-53.
11. Lazarczyk M, Grzela T, Korczak-Kowalska G, Niderla J, Oldak M, Jozwiak J, et al. Pentoxifylline inhibits perforin-dependent natural cytotoxicity in vitro. Oncol Rep. 2002;9:423-6.
12. Correia O, Delgado L, Leal I, Campillo F, Fleming-Torrinha J. Increased interleukin 10, tumor necrosis factor α and interleukin 6 levels in blister fluid of toxic epidermal necrolysis. J Am Acad Dermatol 2002;47:58-62.
13. Parsons J. Toxic epidermal necrolysis. Int J Dermatol. 1992;31;749-68.
14. Tristani-Firouzi P, Petersen M, Saffle J, Morris S, Zone J. Treatment of toxic epidermal necrolysis with intravenous immunoglobulin in children. J Am Acad Dermatol. 2002;47:548-52.
15. Teo L, Tay YK, Liu TT, Kwok C. Stevens-Johnson syndrome and toxic epidermal necrolysis: Efficacy of intravenous immunoglobulin and a review of treatment options. Singapore Med J. 2009;50:29-33.
16. Bastuji-Garin S, Rzany B, Stern RS, Shear NH, Naldi L, Roujeau JC. Clinical classification of cases of toxic epidermal necrolysis, Stevens-Johnson syndrome, and erythema multiforme. Arch Dermatol 1993; 129: 92-6.
17. Chung WH, Hung SI, Yang JY, Su SC, Huang SP, Wei CY et al. Granulysin is a key mediator for disseminated keratinocyte death in Stevens–Johnson syndrome and toxic epidermal necrolysis. Nat Med.2008; 14:1343–50.
18. Posadas SJ, Padial A, Torres MJ, Mayorga C, Leyva L, Sanchez E, et al. Delayed reactions to drugs show levels of perforin, granzyme B, and Fas-L to be related to disease severity. J Allergy Clin Immunol. 2002;109:155–61.
19. 19. Schöpf E, Stühmer A, Rzany B, Victor N, Zentgraf R, Kapp JF. Toxic Epidermal Necrolysis and Stevens-Johnson Syndrome An Epidemiologic Study From West Germany. Arch Dermatol. 1991;127:839–42.
20. Letko E, Papaliodis DN, Papaliodis GN, Daoud YJ, Ahmed AR, Foster CS. Stevens-Johnson syndrome and toxic epidermal necrolysis: a review of the literature. Ann Allergy Asthma Immunol. 2005; 94:419-36.
21. Revuz J, Penso D, Roujeau JC, Guillaume JC, Payne CR, Wechsler J, et al. Toxic epidermal necrolysis. Clinical findings and prognosis factors in 87 patients. Arch Dermatol. 1987;123:1160–5.
22. Bastuji Garin S, Fouchard N, Bertoschi M, Roujeau JC, Revuz J, Wolkenstien P. SCORTEN: A severity-of-illness score for toxic epidermal necrolysis. J Invest Dermatol. 2000;115:149–53.
23. Guégan S, Bastuji-Garin S, Poszepczynska-Guigné E, Roujeau JC, Revuz J. Performance of the SCORTEN during the first five days of hospitalization to predict the prognosis of epidermal necrolysis. J Invest Dermatol 2006;126:272-6
24. Garcia-Doval I, LeCleach L, Bocquet H, Otero XL, Roujeau JC. Toxic epidermal necrolysis and Stevens-Johnson syndrome: does early withdrawal of causative drugs decrease the risk of death? Arch Dermatol. 2000;136:323—7.
25. Schneck J, Fagot JP, Sekula P, Sassolas B, Roujeau JC, Mockenhaupt M. Effects of treatments on the mortality of Stevens-Johnson syndrome and toxic epidermal necrolysis: A retrospective study on patients included in the prospective. EuroSCAR Study. J Am Acad Dermatol. 2008;58:33-40.
26. Redondo P., De Erenchun F.R., Iglesias M.E., Monedero P. Quintanilla E. Toxic epidermal necrolysis. Treatment with pentoxifylline. Br. J. Dermatol.1994; 130: 688-9.
27. Sanclemente G., De la Roche C.A., Escobar C.E., Falabella R. Pentoxifylline in toxic epidermal necrolysis and Stevens-Johnson syndrome. Int. J. Dermatol., 38: 878-9, 1999.
28. Victoria J, Hormaza X. Pentoxifilina en enfermedades catastróficas en niños. Dermatol Pediatr Lat. 2004;2:21-6.
29. Samlaska CP, Winfield EA. Pentoxifylline. J Am Acad Dermatol. 1994;30:603-21.
30. French LE, Trent JT, Kerdel FA. Use of intravenous immunoglobulin in toxic epidermal necrolysis and Stevens-Johnson syndrome: Our current understanding. Int Immunopharmacol. 2006;6:543-9.
31. Prins C, Kerdel FA, Padilla RS, Hunziker T, Chimenti S, Viard I et al. Treatment of toxic epidermal necrolysis with high-dose intravenous immunoglobulins: multi-center retrospective analysis of 48 consecutive cases. Arch Dermatol 2003; 139: 26-32.
32. Halebian P. Improved burn center survival of patients with toxic epidermal necrolysis managed without corticosteroids. Ann Surg. 1986;204:503-12.
33. Roujeau JC, Stern RS. Severe adverse cutaneous reactions to drugs. N Engl J Med. 1994;331:1272-85.
34. Harr T, French LE. Toxic epidermal necrolysis and StevensJohnson syndrome. Orphanet J Rare Dis. 2010;16;39.
How to Cite
Downloads
Downloads
Published
How to Cite
Issue
Section
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |







