Mucormicosis
DOI:
https://doi.org/10.29176/2590843X.302Keywords:
Mucormycosis, mucorales, immunosuppressionAbstract
Mucormycosis is an opportunistic mycosis, uncommonly produced by Zygomycetes fungi of the orderMucorales, associated with immunosuppression, of an aggressive and fatal course. It can be divided into several types, depending on the site of infection, such as rhinocerebral (by extension from the rhinopharynx or by hematogenous dissemination), cutaneous (more commonly in patients with decompensated diabetes mellitus, leukemia or cancer) and pulmonary, among others.
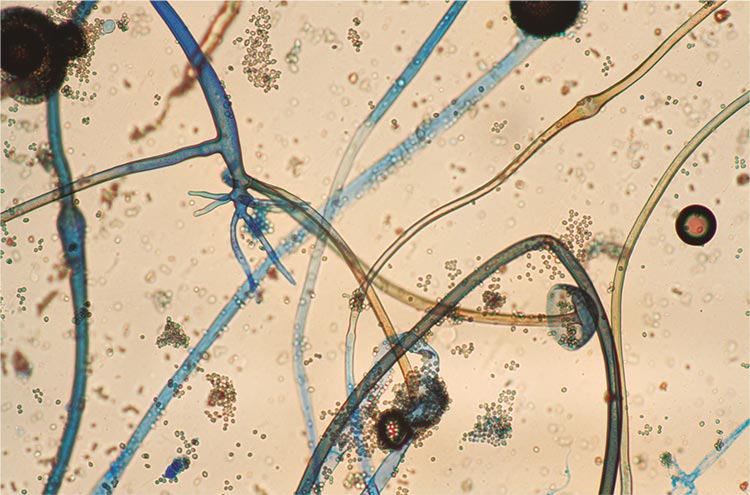
It is generally acquired by the respiratory route since the spores of fungi are found in the environment, although in the primary cutaneous forms, infection is acquired by solution of continuity.
The diagnosis is confirmed by a complete mycological study (direct examination and culture for fungi in Sabouraud agar). The anatomo-pathological study, although it allows visualizing perfectly the mycotic agents, due to its delay is not the method of choice. Once the diagnosis has been made, an early, adequate and appropriate management should be initiated, the predisposing factors identified and corrected promptly, since this entity has a high mortality rate.
Amphotericin B is used as the treatment of choice, which is maintained until the patient is stabilized, and surgical removal of the necrotic material is required in the rhinocerebral or pulmonary varieties. Some authors recommend the use of azoles for these infections, however, in general consensus is that the best treatment is still amphotericin B and the other antifungal drugs are reserved for special cases.
Author Biographies
Nathalie Quiroz
Médica dermatóloga, Universidad del Valle, Cali, Colombia
Janeth del Pilar Villanueva
Médica dermatóloga y micóloga; profesora asistente, Sección de Dermatología y Cirugía Dermatológica, Departamento de Medicina Interna, Facultad de Salud, Universidad del Valle. Cali, Colombia
Edgar Andrés Lozano
Médico dermatólogo, Universidad del Valle, Cali, Colombia
References
Arenas R. Micología médica ilustrada. Cuarta edición. México, D.F.: Editorial McGraw Hill; 2011. p. 251-68.
Cox G. Mucormycosis (zygomycosis). Uptodate. 2015;1-19.
Kwon-Chung KJ. Taxonomy of fungi causing mucormycosis and entomophthoramycosis (zygomycosis) and nomenclature of the disease: Molecular mycologic perspectives. Clin Infect Dis. 2012;54(Suppl.1):S8-15.
https://doi.org/10.1093/cid/cir864
Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, et al. Epidemiology and outcome of zygomycosis: A review of 929 reported cases. Clin Infect Dis. 2005;41:634-53.
https://doi.org/10.1086/432579
Binder U, Maurer E, Lass-Flörl C. Mucormycosis--from the pathogens to the disease. Clin Microbiol Infect. 2014;20(Suppl.6):60-6.
https://doi.org/10.1111/1469-0691.12566
Auberger J, Lass-Florl C, Aigner M, Clausen J, Gastl G, Nachbaur D. Invasive fungal breakthrough infections, fungal colonization and emergence of resistant strains in high-risk patients receiving antifungal prophylaxis with posaconazole: Real-life data from a single-centre institutional retrospective observational study. J Antimicrob Chemother. 2012;67:2268-73.
https://doi.org/10.1093/jac/dks189
Lalwani S, Govindasamy M, Gupta M, Siraj F, Varma V, Mehta N, et al. Gastrointestinal mucormicosis - four cases with different risk factors, involving different anatomical sites. Indian J Gastroenterol. 2012;31:139-43.
https://doi.org/10.1007/s12664-012-0215-z
Ma LJ, Ibrahim AS, Skory C, Grabherr MG, Burger G, Butler M, et al. Genomic analysis of the basal lineage fungus Rhizopus oryzae reveals a whole genome duplication. PLoS Genet. 2009;5:1-11.
https://doi.org/10.1371/journal.pgen.1000549
Morace G, Borghi E. Invasive mold infections: Virulence and pathogenesis of mucorales. Int J Microbiol. 2012;2012;1-5.
https://doi.org/10.1155/2012/349278
Symeonidis AS. The role of iron and iron chelators in zygomycosis. Clin Microbiol Infect. 2009;15(Suppl.5):26-32.
https://doi.org/10.1111/j.1469-0691.2009.02976.x
Ibrahim AS, Spellberg B, Avanessian V, Fu Y, Edwards JE Jr. Rhizopus oryzae adheres to, is phagocytosed by and damages endothelial cells in vitro. Infect Immun. 2005;73:778-83.
https://doi.org/10.1128/IAI.73.2.778-783.2005
Mingfu L, Spellberg B, Phan QT, Fu Y, Fu Y, Lee AS, et al. The endothelial cell receptor GRP78 is required for mucormycosis pathogenesis in diabetic mice. J Clin Invest. 2010;120:1914-24.
https://doi.org/10.1172/JCI42164
Levitz SM, Selsted ME, Ganz T, Lehrer RI, Diamond RD. In vitro killing of spores and hyphae of Aspergillus fumigatus and Rhizopus oryzae by rabbit neutrophil cationic peptides and bronchoalveolar macrophages. J Infect Dis. 1986;154:483-9.
https://doi.org/10.1093/infdis/154.3.483
Netea MG, Ferwerda G, van der Graaf CA, van der Meer JW, Kullberg BJ. Recognition of fungal pathogens by toll-like receptors. Curr Pharm Des. 2006;12:4195-201.
https://doi.org/10.2174/138161206778743538
Netea MG, van der Meer JW, Kullberg BJ. Role of the dual interaction of fungal pathogens with pattern recognition receptors in the activation and modulation of host defense. Clin Microbiol Infect. 2006;12:404-9.
https://doi.org/10.1111/j.1469-0691.2006.01388.x
Chamilos G, Lewis RE, Lamaris G, Walsh TJ, Kontoyiannis DP. Zygomycetes hyphae trigger an early, robust pro-inflammatory response in human polymorphonuclear neutrophils through toll-like receptor 2 induction but display relative resistance to oxidative damage. Antimicrob Agents Chemother. 2008;52:722-4.
https://doi.org/10.1128/AAC.01136-07
van de Veerdonk FL, Kullberg BJ, van der Meer JW, Gow NA, Netea MG. Host-microbe interactions: Innate pattern recognition of fungal pathogens. Curr Opin Microbiol. 2008;11:305-12.
https://doi.org/10.1016/j.mib.2008.06.002
Warris A, Netea MG, Verweij PE, Gaustad P, Kullberg BJ, Weemaes CM, Abrahamsen TG. Cytokine responses and regulation of interferon-gamma release by human mononuclear cells to Aspergillus fumigatus and other filamentous fungi. Med Mycol. 2005;43:613-21.
https://doi.org/10.1080/13693780500088333
Lewis RE, Kontoyiannis DP. Epidemiology and treatment of mucormycosis. Future Microbiol. 2013;8:1163-75.
https://doi.org/10.2217/fmb.13.78
Spellberg B, Edwards J, Jr, Ibrahim A. Novel perspectives on mucormycosis: Pathophysiology, presentation, and management. Clin Microbiol Rev. 2005;18:556-69.
https://doi.org/10.1128/CMR.18.3.556-569.2005
Geramizadeh B, Modjalal M, Nabai S, Banani S, Abbas F, Hamidreza F, et al. Gastrointestinal zygomycosis: A report of three cases. Mycopathologia. 2007;164:35-8.
https://doi.org/10.1007/s11046-007-9022-y
Kontoyiannis DP, Wessel VC, Bodey GP, Rolston KV. Zygomycosis in the 1990s in a tertiary-care cancer center. Clin Infect Dis. 2000;30:851-6.
https://doi.org/10.1086/313803
Kauffman CA, Malani AN. Zygomycosis: An emerging fungal infection with new options for management. Curr Infect Dis Rep. 2007;9:435-40.
https://doi.org/10.1007/s11908-007-0066-4
Kontoyiannis DP, Lionakis MS, Lewis RE, Chamilos G, Healy M, Perego C, et al. Zygomycosis in a tertiary-care cancer center in the era of Aspergillus-active antifungal therapy: A case-control observational study of 27 recent cases. J Infect Dis. 2005;191:1350-60.
https://doi.org/10.1086/428780
Trifilio SM, Bennett CL, Yarnold PR, McKoy JM, Parada J, Mehta J, et al. Breakthrough zygomycosis after voriconazole administration among patients with hematologic malignancies who receive hematopoietic stem-cell transplants or intensive chemotherapy. Bone Marrow Transplant. 2007;39:425-9.
https://doi.org/10.1038/sj.bmt.1705614
Lanternier F, Sun HY, Ribaud P, Singh N, Kontoyiannis DP, Lortholary O. Mucormycosis in organ and stem cell transplant recipients. Clin Infect Dis. 2012;54:1629-32.
https://doi.org/10.1093/cid/cis195
Almyroudis NG, Sutton DA, Linden P, Rinaldi MG, Fung J, Kusne S. Zygomycosis in solid organ transplant recipients in a tertiary transplant center and review of the literature. Am J Transplant. 2006;6:2365-74.
https://doi.org/10.1111/j.1600-6143.2006.01496.x
Aslani J, Eizadi M, Kardavani B, Khoddami-Vishteh HR, Nemati E, Hoseini SM, Einollahi B. Mucormycosis after kidney transplantations: Report of seven cases. Scand J Infect Dis. 2007;39:703-6.
https://doi.org/10.1080/00365540701299590
Singh N, Aguado JM, Bonatti H, Forrest G, Gupta KL, Safdar N, et al. Zygomycosis in solid organ transplant recipients: A prospective, matched case-control study to assess risks for disease and outcome. J Infect Dis. 2009;200:1002-11.
https://doi.org/10.1086/605445
Ibrahim AS, Spellberg B, Edwards J, Jr. Iron acquisition: A novel perspective on mucormycosis pathogenesis and treatment. Curr Opin Infect Dis. 2008;21:620-5.
https://doi.org/10.1097/QCO.0b013e3283165fd1
Maertens J, Demuynck H, Verbeken EK, Zachée P, Verhoef GE, Vandenberghe P, Boogaerts MA. Mucormycosis in allogeneic bone marrow transplant recipients: Report of five cases and review of the role of iron overload in the pathogenesis. Bone Marrow Transplant. 1999;24:307-12.
https://doi.org/10.1038/sj.bmt.1701885
Lanternier F, Dannaoui E, Morizot G, Elie C, García-Hermoso D, Huerre M, et al. A global analysis of mucormycosis in France: The RetroZygo Study (2005-2007). Clin Infect Dis. 2012;54(Suppl.1):35-43.
https://doi.org/10.1093/cid/cir880
Andresen D, Donaldson A, Choo L, Knox A, Klaassen M, Ursic C, et al. Multifocal cutaneous mucormycosis complicating polymicrobial wound infections in a tsunami survivor from Sri Lanka. Lancet. 2005;365:876-8.
https://doi.org/10.1016/S0140-6736(05)71046-1
Kouadio IK, Aljunid S, Kamigaki T, Hammad K, Oshitani H. Infectious diseases following natural disasters: Prevention and control measures. Expert Rev Anti Infect Ther. 2012;10:95-104.
https://doi.org/10.1586/eri.11.155
Neblett-Fanfair R, Benedict K, Bos J, Bennett SD, Lo YC, Adebanjo T, et al. Necrotizing cutaneous mucormycosis after a tornado in Joplin, Missouri, in 2011. N Engl J Med. 2012;367:2214-25.
https://doi.org/10.1056/NEJMoa1204781
Kurosawa M, Yonezumi M, Hashino S, Tanaka J, Nishio M, Kaneda M, et alet al. Epidemiology and treatment outcome of invasive fungal infections in patients with hematological malignancies. Int J Hematol. 2012;96:748-57.
https://doi.org/10.1007/s12185-012-1210-y
Marty FM, Cosimi LA, Baden LR. Breakthrough zygomycosis after voriconazole treatment in recipients of hematopoietic stem-cell transplants. N Engl J Med. 2004;350:950-2.
https://doi.org/10.1056/NEJM200402263500923
Oren I. Breakthrough zygomycosis during empirical voriconazole therapy in febrile patients with neutropenia. Clin Infect Dis. 2005;40:770-1.
https://doi.org/10.1086/427759
Gale GR, Welch AM. Studies of opportunistic fungi. I. Inhibition of Rhizopus oryzae by human serum. Am J Med Sci. 1961;241:604-12.
https://doi.org/10.1097/00000441-196105000-00008
Teixeira CA, Medeiros PB, Leushner P, Almeida F. Rhinocerebral mucormycosis: Literature review a propôs of a rare entity. BMJ Case Rep. 2013:2013:1-3.
https://doi.org/10.1136/bcr-2013-008552
Rajagopalan S. Serious infections in elderly patients with diabetes mellitus. Clin Infect Dis. 2005;40:990-6.
https://doi.org/10.1086/427690
Tedder M, Spratt JA, Anstadt MP, Hegde SS, Tedder SD, Lowe JE. Pulmonary mucormycosis: Results of medical and surgical therapy. Ann Thorac Surg. 1994;57:1044-50.
https://doi.org/10.1016/0003-4975(94)90243-7
Brown RB, Johnson JH, Kessinger JM, Sealy WC. Bronchovascular mucormycosis in the diabetic: An urgent surgical problem. Ann Thorac Surg. 1992;53:854-5.
https://doi.org/10.1016/0003-4975(92)91450-N
Murphy RA, Miller WT, Jr. Pulmonary mucormycosis. Semin Roentgenol. 1996;31:83-7.
https://doi.org/10.1016/S0037-198X(96)80043-5
Chamilos G, Marom EM, Lewis RE, Lionakis MS, Kontoyiannis DP. Predictors of pulmonary zygomycosis versus invasive pulmonary aspergillosis in patients with cancer. Clin Infect Dis. 2005;41:60-6.
https://doi.org/10.1086/430710
Adam RD, Hunter G, DiTomasso J, Comerci G, Jr. Mucormycosis: Emerging prominence of cutaneous infections. Clin Infect Dis. 1994;19:67-76.
https://doi.org/10.1093/clinids/19.1.67
Cocanour CS, Miller-Crotchett P, Reed RL 2nd, Johnson PC, Fischer RP. Mucormycosis in trauma patients. J Trauma. 1992;32:12-5
https://doi.org/10.1097/00005373-199201000-00003
Warkentien T, Rodríguez C, Lloyd B, Wells J, Weintrob A, Dunne JR, et al. Invasive mold infections following combat related injuries. Clin Infect Dis. 2012;55:1441-9.
https://doi.org/10.1093/cid/cis749
Chakrabarti A, Kumar P, Padhye AA, Chatha L, Singh SK, Das A, et al. Primary cutaneous zygomycosis due to Saksenaea vasiformis and Apophysomyces elegans. Clin Infect Dis. 1997;24:580-3.
https://doi.org/10.1093/clind/24.4.580
Weinberg WG, Wade BH, Cierny G 3rd, Stacy D, Rinaldi MG. Invasive infection due to Apophysomyces elegans in immunocompetent hosts. Clin Infect Dis. 1993;17:881-4.
https://doi.org/10.1093/clinids/17.5.881
Arnáiz-García ME, Alonso-Peña D, González-Vela MC, García-Palomo JD, Sanz-Giménez-Rico JR, Arnáiz-García AM.Cutaneous mucormycosis: Report of five cases and review of the literature. J Plast Reconstr Aesthet Surg. 2009;62:434-41.
https://doi.org/10.1016/j.bjps.2008.04.040
Geisen M, Fodor P, Eich G, Zollinger A, Dzemali O, Blumenthal S. Disseminated cutaneous mucormycosis in a patient on high-dose steroid therapy for severe ARDS. Intensive Care Med. 2011;37:1895-6.
https://doi.org/10.1007/s00134-011-2347-5
Ismail MH, Hodkinson HJ, Setzen G, Sofianos C, Hale MJ. Gastric mucormycosis. Trop Gastroenterol. 1990;11:103-5.
Oliver MR, van Voorhis WC, Boeckh M, Mattson D, Bowden RA. Hepatic mucormycosis in a bone marrow transplant recipient who ingested naturopathic medicine. Clin Infect Dis. 1996;22:521-4.
https://doi.org/10.1093/clinids/22.3.521
Agha FP, Lee HH, Boland CR, Bradley SF. Mucormycoma of the colon: Early diagnosis and successful management. AJR Am J Roentgenol. 1985;145:739-41.
https://doi.org/10.2214/ajr.145.4.739
Prasad N, Ram R, Satti Reddy V, Dakshinamurty KV. Nonfatal gastric mucormycosis in a renal transplant recipient. South Med J. 1997;90:341-4.
https://doi.org/10.1097/00007611-199703000-00017
Hosseini M, Lee J. Gastrointestinal mucormycosis mimicking ischemic colitis in a patient with systemic lupus erythematosus. Am J Gastroenterol. 1998;93:1360-2.
https://doi.org/10.1111/j.1572-0241.1998.00417.x
Levy E, Bia MJ. Isolated renal mucormycosis: Case report and review. J Am Soc Nephrol. 1995;5:2014-9.
Nagy-Agren SE, Chu P, Smith GJ, Waskin HA, Altice FL. Zygomycosis (mucormycosis) and HIV infection: Report of three cases and review. J Acquir Immune Defic Syndr Hum Retrovirol. 1995;10:441-9.
https://doi.org/10.1097/00042560-199512000-00007
Weng DE, Wilson WH, Little R, Walsh TJ. Successful medical management of isolated renal zygomycosis: Case report and review. Clin Infect Dis. 1998;26:601-5.
https://doi.org/10.1086/514562
Langston C, Roberts DA, Porter GA, Bennett WM. Renal phycomycosis. J Urol. 1973;109:941-4.
https://doi.org/10.1016/S0022-5347(17)60587-1
Melnick JZ, Latimer J, Lee El, Henrich WL. Systemic mucormycosis complicating acute renal failure: Case report and review of the literature. Ren Fail. 1995;17:619-627
https://doi.org/10.3109/08860229509037628
Tedder M, Spratt JA, Anstadt MP, Hegde SS, Tedder SD, Lowe JE. Pulmonary mucormycosis: Results of medical and surgical therapy. Ann Thorac Surg. 1994;57:1044-50.
https://doi.org/10.1016/0003-4975(94)90243-7
Brown RB, Johnson JH, Kessinger JM, Sealy WC. Bronchovascular mucormycosis in the diabetic: An urgent surgical problem. Ann Thorac Surg. 1992;53:854-5.
https://doi.org/10.1016/0003-4975(92)91450-N
González CE, Couriel DR, Walsh TJ. Disseminated zygomycosis in a neutropenic patient: Successful treatment with amphotericin B lipid complex and granulocyte colony-stimulating factor. Clin Infect Dis. 1997;24:192-6.
https://doi.org/10.1093/clinids/24.2.192
Chamilos G, Lewis RE, Kontoyiannis DP. Delaying amphotericin B-based frontline therapy significantly increases mortality among patients with hematologic malignancy who have zygomycosis. Clin Infect Dis.2008;47:503-9.
https://doi.org/10.1086/590004
Noxafil (posaconazole). Highlights of prescribing information. Fecha de consulta: 18 de marzo de 2014. Disponible en:https://www.merck.com/product/usa/pi_circulars/n/noxafil/noxafil_pi.pdf.
How to Cite
Downloads
Downloads
Published
How to Cite
Issue
Section
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |







