Aspectos moleculares, inmunológicos y patogénicos de la infección por el virus del papiloma humano (VPH)
Keywords:
VPH, biología molecular, inmunología, patogénesisAbstract
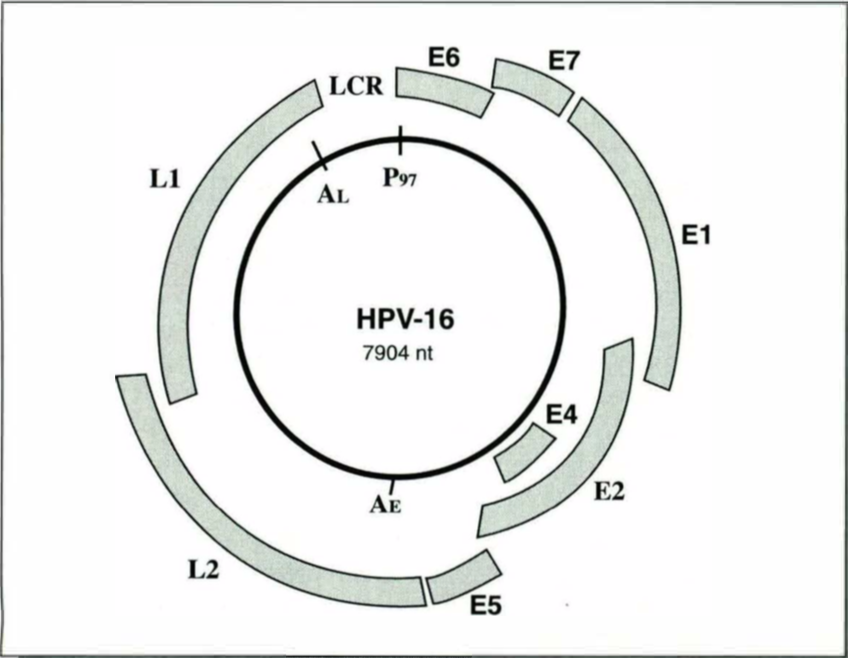
Hasta el momento se han identificado más de 80 genotipos del VPH. La importancia de estos virus se debe tanto a su potencial de transformación maligna como a su alta prevalencia y distribución en el mundo. Se presenta una revisión de la biología molecular, inmunología y patogénesis del VPH, con énfasis en los genotipos asociados con infección genital.
Author Biography
Gloria Sanclemente Mesa, Universidad de Antioquia
Profesora de Dermatología, Universidad de Antioquia, Medellín.
References
2. Zur Hausen H, de Villiers E-M. Human papillomaviruses. Annu Rev Microbiol 1994; 48:427-447.
https://doi.org/10.1146/annurev.mi.48.100194.002235
3. DiMaio D, Neary K. The genetics of bovine papillomavirus type 1. En: Pfister H (ed}. Papillomaviruses and human cancer. CRC Press, Boca Raton 1990 pp: 113.
4. Fuchs PG, Pfister H. Molecular biology of HPV and mechanisms of keratinocyte transformation. En: Gross G, von Krogh G (eds.). Human papillomavirus infections in dermatovenereology, CRC Press, Boca Raton, USA 1997 pp. 15-46.
5. Shah KV, Howley PM. Papilllomaviruses. En: Fields BN, Knipe DM (eds.). Fields Virology, 2a. ed. New York: Raven Press, 1990, pp. 1625-1650.
6. Beutner KR, Tyring S. Human papillomavirus and human disease. Am J Med 1997; 102:9-15.
https://doi.org/10.1016/S0002-9343(97)00178-2
7. Anderson B, Hariri A, Pittelkow MR et al. Characte risation of SKn-1a/1 POU domain factors and linkage to papillomavirus gene expression. J Biol Chem 1997; 272:15905.
https://doi.org/10.1074/jbc.272.25.15905
8. Saunders N, Frazer IH. Simplifying the molecular mechanisms of human papillomavirus. Dermatol Clin 1998; 16:823-827.
https://doi.org/10.1016/S0733-8635(05)70054-1
9. Brescia RJ, Jenson AS, Lancaster WD et al. The role of human papillomaviruses in the pathogenesis and histologic classification of precancerous lesions of the cervix. Human Pathol 1986; 17:552-559.
https://doi.org/10.1016/S0046-8177(86)80126-5
10. Howley PM. Papillomaviridae: The viruses and their replication. En: Fields BN, Knipe DM, Howley PM. (eds.) Fundamental Virology, 3a. ed. Lippincott-Raven, Philadelphia 1996; pp. 947-978.
11. Cobb MW. Human papillomavirus infection. J Am Acad Dermatol 1990; 22:547-566.
https://doi.org/10.1016/0190-9622(90)70073-Q
12. Briggaman RA, Wheeler CE Jr. lmmunology of human warts. J Am Acad Dermatol 1979; 1:297-304.
https://doi.org/10.1016/S0190-9622(79)70022-3
13. Grussendorf-Conen El. Warts and HPV-related squa mous cell tumors of the skin. En: Human papilloma virus infections in dermatovenereology, CRC Press lnc, 1997; pp. 117-130.
14. Lorincz AT, Reid R, Jenson AB, et al. Human papillomavirus infection of the cervix: relative risk associations of 15 common anogenital types. Obstet Gynecol 1992; 79:328-337.
https://doi.org/10.1097/00006250-199203000-00002
15. Anon. Sexually transmitted diseases quarterly report: genital warts and genital herpes simplex virus infections in England and Wales. Commun Dis Rep COR Weekly 1997; 7:310-312.
16. Persson G, Andersson K, Krantz l. Symptomatic genital papillomavirus infection in a community-incidence and clinical picture. Acta Obstet Gynecol Scand 1996; 75:287-290.
https://doi.org/10.3109/00016349609047103
17. Koutsky L. Epidemiology of genital human papillomavirus infection. Am J Med 1997; 102:3-8.
https://doi.org/10.1016/S0002-9343(97)00177-0
18. Kataja V, Syrjanen S, Yliskoski M et al. Risk factors associated with cervical human papillomavirus infection: a case control study. Am J Epidemiol 1993; 138:735-745.
https://doi.org/10.1093/oxfordjournals.aje.a116911
19. Daling JR, Sherman KJ, Weiss NS. Risk factors for condyloma acuminatum in women. Sex Transm Dis 1986; 13:16-18.
https://doi.org/10.1097/00007435-198601000-00004
20. Munk C, Svare El, Poli P, et al. History of genital warts in 10,838 women 20 to 29 years of age from the general population: Risk factors and association with Papanicolaou smear history. Sex Trans Dis 1997; 24:567-572.
https://doi.org/10.1097/00007435-199711000-00003
21. Durst M, Kleinheinz A, Hotz M, et al. The physical state of human papillomavirus type 16 DNA in benign and malignant genital tumors. J Gen Virol 1985; 66:1515-1522.
https://doi.org/10.1099/0022-1317-66-7-1515
22. Antinore MJ, Birrer MJ, Patel D, et al. The human papillomavirus type 16 E7 gene product interacts with and trans-activates the AP1 family of transcription factors. EMBO J 1996;15:1950-1960.
https://doi.org/10.1002/j.1460-2075.1996.tb00546.x
23. Bosch et al. Prevalence of HPV in cervical cancer- a worldwide perspective. J Natl Cancer lnst 1995; 81:796.
https://doi.org/10.1093/jnci/87.11.796
24. Zaki SR, Judd R, Coffield LM, et al. Human papillomavirus infection and anal carcinoma. Retrospective analysis by in sítu hybridization and the polymerase chain reaction. Am J Pathol 1992; 140:1345-1355.
25. McKenna 08, O'Connor D, Kay E, et al. The role of human papilloma virus in skin cancer- current status. J Eur Acad Dermatol Venereol 1997; 9:103-11O.
https://doi.org/10.1111/j.1468-3083.1997.tb00246.x
26. Moy R, Elizieri Y. Significance of human papillomavirus-induced squamous cell carcinoma to dermatologists. Arch Dermatol 1994; 130:235-238.
https://doi.org/10.1001/archderm.1994.01690020101017
27. Bryan JT, Stoler MH, Tyring SK, et al. High-grade dysplasia in genital warts from two patients infected with the human immunodeficiency virus. J Med Viral 1998; 54:69-73.
https://doi.org/10.1002/(SICI)1096-9071(199801)54:1<69::AID-JMV10>3.0.CO;2-Z
28. Orth G, Jablonska S, Jarzabek-Chorzelska M, et al. Characteristics of the lesions and risk of malignant conversion as related to the type of the human papillomavirus involved in epidermodysplasia verruciformis. Cancer Res 1979; 39:1074-1079.
29. Friis S, Kjaer SK, Frisch M, et al. Cervical intraepithelial neoplasia, anogenital cancer, and other cancer types in women after hospitalization for condylomata acuminata. J lnfect Dis 1997; 175:743-748.
https://doi.org/10.1086/513966
30. Gissmann L, Wolnik L, lkenberg H, et al. Human papillomavirus types 6 and 11 DNA sequences in ge nital and laryngeal papillomas and in sorne cervical cancers. Proc Natl Acad Sci USA 1983; 80:560-563.
https://doi.org/10.1073/pnas.80.2.560
31. Shamanin V, zur Hausen H, Lavergne O, et al. Human papillomavirus infections in non-melanoma skin cancers from renal transplant recipients and non-immunosuppressed patients. J Natl Cancer lnst 1996; 88:802-811 .
https://doi.org/10.1093/jnci/88.12.802
32. Shwartz RA. Verrucous carcinoma of the skin and mucosa. J Am Acad Dermatol 1995; 32:1-21.
https://doi.org/10.1016/0190-9622(95)90177-9
33. Ranst MV, Tachezy R, Delius H,et al. Classification of the human papillomaviruses based on their molecular evolutionary relationship. En: Gross G., Krogh GV. (eds) Human papillomavirus infections in dermatovenereology, CRC Press, Boca Raton, Florida, USA, 1997 pp. 69:82.
34. Van Ranst M, Tachezy R, Burk RO. Human papillomaviruses: A neverending story?. En: Lacey C. Papillomavirus reviews: current research on papillomaviruses, Leeds University Press, Leeds, 1996 pp. 1-19.
35. Zur Hausan H. Human papillomavirus in human cancer. Cancer 1987; 59:1690-1692.
https://doi.org/10.1002/1097-0142(19870515)59:10<1692::AID-CNCR2820591003>3.0.CO;2-F
36. Moy RL,Eliezri YO, Nuovo GJ,et al. Human papillomavirus type 16 DNA periungueal squamous cell carcinoma. J Am Med Assoc 1989; 261:2669-2673.
https://doi.org/10.1001/jama.1989.03420180093037
37. Sau P, McMarlin SL, Sperling LC, et al. Bowen's disease of the nail bed and periungueal area. Arch Dermatol 1994; 130:204-209.
https://doi.org/10.1001/archderm.1994.01690020070012
38. Masih AS, Stoler MH, Farrow GM, et al. Human papillomavirus in penile squamous cell lesions: A comparison of an isotopic RNA and two commercial nonisotopic DNA in situ hybridization methods. Arch Pathol Lab Med 1993; 117:302-307.
39. Turazza E, Lapena A, Sprovieri O, et al. Low-risk human papillomavirus types 6 and 11 associated with carcinomas of the genital and upper aero-digestive trae!. Acta Obstet Gynecol Scand 1997; 76:271-276.
https://doi.org/10.3109/00016349709047808
40. Sonnex C, Scholefield JH, Kocjan G, et al. Anal human papillomavirus infection in heterosexuals with genital warts: prevalence and relation with sexual behavior. BMJ 1991; 303:1243.
https://doi.org/10.1136/bmj.303.6812.1243
41. Rymark P, Forslund O, Hansson BG, et al. Genital HPV infection not a local but a regional infection: experience from a female teenage group. Genitourin Med 1993; 69:18-22.
https://doi.org/10.1136/sti.69.1.18
42. Chopra KF, Tyring SK. The impact of the human immunodeficiency virus on the human papillomavirus epidemic. Arch Dermatol 1997; 133:629-633.
https://doi.org/10.1001/archderm.1997.03890410085011
43. Critchlow CW, Surawicz CM, Holmes KK et al. Prospective study of high grade anal squamous intraepithelial neoplasia in a cohort of homosexual men: lnfluence of HIV infection, immunosuppression and human papillomavirus infection. AIDS 1995; 9:1255-1262.
https://doi.org/10.1097/00002030-199511000-00007
44. Streilen JW. Skin-associated lymphoid tissues (SALT): origins and functions. J lnvest Dermatol 1983; 80:12S-16S.
https://doi.org/10.1111/1523-1747.ep12536743
45. Bos JO, Kapsenberg ML. The skin immune system: lts cellular constituents and their interactions. lmmunol Today 1986; 7:235-240 .
https://doi.org/10.1016/0167-5699(86)90111-8
46. Nickoloff BJ. Dermal immune system. CRC Press, Boca Raton, 1993.
47. Cerio R, Griffiths CEM, Cooper KD et al. Characterization of factor XIlla positive dermal dendritic cells in normal and inflamed skin. Br J Dermatol 1989; 121:421-431.
https://doi.org/10.1111/j.1365-2133.1989.tb15509.x
48. Sepulveda-Merril C, Mayall S, Hamblin AS, et al. Antigen presenting capacity in normal human dermis is mainly subserved by CD1a+ cells. Br J Dermatol 1994; 131:15-22.
https://doi.org/10.1111/j.1365-2133.1994.tb08451.x
49. Barker JNWN, Mitra RS, Griffiths CEM, et al. Keratinocytes as initiators of inflammation. Lancet 1991; 337:211-214.
https://doi.org/10.1016/0140-6736(91)92168-2
50. Frazer IH. The role of the immune system in ano-genital human papillomavirus. Austr J Dermatol 1998; 39(suppl.):S5-S7.
51. Frazer IH. lmmunology of papillomavirus infection. Curr Opin lmmunol 1996; 8:484-491.
https://doi.org/10.1016/S0952-7915(96)80035-5
52. Coleman N, Birley HDL, Rentan AM, et al. lmmunological events in regressing genital warts. Am J Clin Pathol 1994; 102:768-774.
https://doi.org/10.1093/ajcp/102.6.768
53. Malejczyk J, Malejczyk M, Kock A et al. Autocrine growth limitation of human papillomavirus type 16-harboring keratinocytes by constitutively released tumor necrosis factor-a. J lmmunol 1992; 149:2702-2708.
54. Han R, Breitburd F, Marche PN, et al. Linkage of regression and malignant conversion of rabbit viral papillomas to MHC class II genes. Nature 1992; 356:66-68. Breathnach SM. The Langerhans Cell. Br J Dermatol 1988; 119:463-469.
https://doi.org/10.1111/j.1365-2133.1988.tb03249.x
56. Berman B, Chen VL, France DS, et al, Anatomical mapping of epidermal Langerhans cell densities in adults. Br J Dermatol 1983; 109:553-558.
https://doi.org/10.1111/j.1365-2133.1983.tb07678.x
57. Misery L, Dezutter-Dambuyant C. Precursors of Langerhans cells. J Eur Acad Dermatol Venereol 1995; 5:124-131.
https://doi.org/10.1111/j.1468-3083.1995.tb00531.x
58. Grebbe S, Bruvers S, Granstein RD. Effects of immunomodulatory cytokines on the presentation of tu- mor-associated antigens by epidermal Langerhans cells. J lnvest Dermatol 1992; 99:66S-68S.
https://doi.org/10.1111/1523-1747.ep12669018
59. Sprecher E, Becker Y. Dendritic cells in the epidermis and the lymph nodes-A Review. En: Becker Y (ed). Skin Langerhans (dendritic) cells in virus infections and AIDS. Kluwer Academi Publishers, USA 1991 pp. 3-23.
https://doi.org/10.1007/978-1-4615-3942-1_1
60. Wang B, Amerio P, Sauder DN. Role of cytokines in epidermal Langerhans cell migration. J Leukoc Biol 1999; 66:33-39.
https://doi.org/10.1002/jlb.66.1.33
61. Morris HH, Gatter KC, Sykes G, et al. Langerhans cells in human cervical epithelium: Effects of wart virus infection and intraepithelial neoplasia. Br J Obstet Gynaecol 1983; 90:412-420.
https://doi.org/10.1111/j.1471-0528.1983.tb08936.x
62. Chardonet Y, Viac J, Thivolet J. Langerhans cells in human warts. Br J Dermatol 1986; 115:669-675.
https://doi.org/10.1111/j.1365-2133.1986.tb06647.x
63. Jenson AB, Kurman RJ, Lancaster WD. Tissue effects of and host response to human papillomavirus infection. Dermatol Clin 1991; 9:203-209.
https://doi.org/10.1016/S0733-8635(18)30410-8
64. Mota F, Rayment N, Chong S, et al. The antigen presenting environment in normal and human papillomavirus (HPV)-related premalignant cervical epithelium. Clin Exp lmmunol 1999; 116:33-40.53. Malejczyk J, Malejczyk M, Kock A et al. Autocrine growth limitation of human papillomavirus type 16-harboring keratinocytes by constitutively released tumor necrosis factor-a. J lmmunol 1992; 149:2702-2708.
https://doi.org/10.1046/j.1365-2249.1999.00826.x
54. Han R, Breitburd F, Marche PN, et al. Linkage of regression and malignant conversion of rabbit viral papillomas to MHC class II genes. Nature 1992; 356:66-68. Breathnach SM. The Langerhans Cell. Br J Dermatol 1988; 119:463-469.
https://doi.org/10.1111/j.1365-2133.1988.tb03249.x
56. Berman B, Chen VL, France DS, et al, Anatomical mapping of epidermal Langerhans cell densities in adults. Br J Dermatol 1983; 109:553-558.
https://doi.org/10.1111/j.1365-2133.1983.tb07678.x
57. Misery L, Dezutter-Dambuyant C. Precursors of Langerhans cells. J Eur Acad Dermatol Venereol 1995; 5:124-131.
https://doi.org/10.1111/j.1468-3083.1995.tb00531.x
58. Grebbe S, Bruvers S, Granstein RD. Effects of immu- nomodulatory cytokines on the presentation of tu- mor-associated antigens by epidermal Langerhans cells. J lnvest Dermatol 1992
https://doi.org/10.1111/1523-1747.ep12669018
99:66S-68S. Sprecher E, Becker Y. Dendritic cells in the epider- mis and the lymph nodes-A Review. En: Becker Y (ed). Skin Langerhans (dendritic) cells in virus infec- tions and AIDS. Kluwer Academi Publishers, USA 1991 pp. 3-23.
https://doi.org/10.1007/978-1-4615-3942-1_1
60. Wang B, Amerio P, Sauder DN. Role of cytokines in epidermal Langerhans cell migration. J Leukoc Biol 1999; 66:33-39.
https://doi.org/10.1002/jlb.66.1.33
61. Morris HH, Gatter KC, Sykes G, et al. Langerhans cells in human cervical epithelium: Effects of wart virus infection and intraepithelial neoplasia. Br J Obstet Gynaecol 1983; 90:412-420.
https://doi.org/10.1111/j.1471-0528.1983.tb08936.x
62. Chardonet Y, Viac J, Thivolet J. Langerhans cells in human warts. Br J Dermatol 1986; 115:669-675.
https://doi.org/10.1111/j.1365-2133.1986.tb06647.x
63. Jenson AB, Kurman RJ, Lancaster WD. Tissue effects of and host response to human papillomavirus infection. Dermatol Clin 1991; 9:203-209.
https://doi.org/10.1016/S0733-8635(18)30410-8
64. Mota F, Rayment N, Chong S, et al. The antigen- presenting environment in normal and human papillo- mavirus (HPV)-related premalignant cervical epithe- lium. Clin Exp lmmunol 1999; 116:33-40.
https://doi.org/10.1046/j.1365-2249.1999.00826.x
65. Bhawan J, Dayal Y, Bhan AK. Langerhans cells in molluscum contagiosum, verruca vulgaris, plantar wart, and condyloma acuminatum. J Am Acad Dermatol 1986; 15:645-649.
https://doi.org/10.1016/S0190-9622(86)70219-3
66. Chardonnet Y, Viac J, Thivolet J. Langerhans cells in human warts. Br J Dermatol 1986; 115:669-675.
https://doi.org/10.1111/j.1365-2133.1986.tb06647.x
67. Drijkoningen M, De Wolf-Peeters C, Degreef H, et al. Epidermal Langerhans cells, dermal dendritic cells, and keratinocytes in viral lesions of skin and mucous membranes: an immunohistochemical study. Arch Dermatol Res 1988; 280:220-227.
https://doi.org/10.1007/BF00513961
68. Morelli AE, Belardi G, DiPaola G, et al. Cellular subsets and epithelial ICAM-1 and HLA-DR expre- ssion in human papillomavirus infection of the vulva. Acta Derm Venereol 1994 ; 74:45-50.
69. Memar OM, Arany 1, Tyring SK. Skin-associated lymphoid tissue in human immunodeficiency virus-1, human papillomavirus, and herpes simplex virus infections. J lnvest Dermatol 1995; 105: 99S-104S.
https://doi.org/10.1038/jid.1995.20
70. Tyring SK, Arany 1, Stanley MA, et al. Stimulation of local cytokine and cell mediated immune responses in human papillomavirus (HPV) patients receiving lmiquimod. (Poster #0221). lnternational Congress of Sexually Transmitted Diseases (ISSTDR). Sevilla, España octubre 1997.
71. Kupper TS. Mechanisms of cutaneous inflammation:interactions between epidermal cytokines, adhesion molecules, and leukocytes. Arch Dermatol 1989; 125:1406-1412.
https://doi.org/10.1001/archderm.1989.01670220102017
72. Albanesi C, Cavani A, Girolomoni G. IL-17 is produced by nickel-specific T lymphocytes and regulates ICAM-1 expression and chemokine production in human keratinocytes: Synergistic or antagonist effects with IFN-a and TNF-a. J lmmunol 1999; 162:494-502. Schreiber S, Kilgus O, Kutil R, et al. Cytokine pattern of Langerhans cells isolated from murine epidermal cell cultures. J lmmunol 1992; 149:3525-3534.
74. Majewski S, Malejczyk J, Jablonska S. The role of cytokines and other factors in HPV infection and HPV- associated tumors. Papillomavirus Report 1996; 7:143-154.
How to Cite
Downloads
Downloads
Published
How to Cite
Issue
Section
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |






