Procesamiento de biopsias de piel en el laboratorio de patología
DOI:
https://doi.org/10.29176/2590843X.278Palabras clave:
biopsia, laboratorio, dermatopatología, márgenes de resecciónResumen
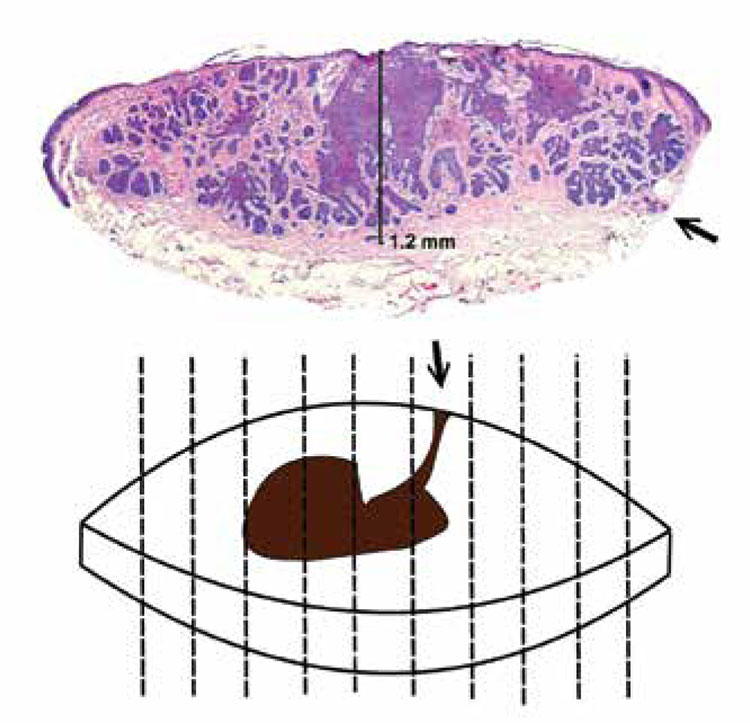
El procesamiento de las biopsias de piel es el primer paso en el que interviene el dermatopatólogo. Este importante evento es a menudo delegado en personal escasamente entrenado, como auxiliares o estudiantes de posgrado en sus primeros años de formación. Las consecuencias de esta acción son generalmente irreversibles y habitualmente los errores cometidos no pueden repararse.
Biografía del autor/a
Wilber Javier Martínez
Médico patólogo, especialista en Dermatopatología y en Gerencia de IPS, profesor de Dermatopatología Universidad Autónoma de Bucaramanga, Bucaramanga, Colombia.
Rodrigo Restrepo
Médico dermatopatólogo, jefe programa de especialización en Dermatopatología Universidad CES, profesor de Dermatopatología Universidad Pontificia Bolivariana, Medellín, Colombia.
Referencias bibliográficas
2. Martin RC, Scoggins CR, Ross MI, Reintgen DS, Noyes RD, Edwards MJ, et al. Is incisional biopsy of melanoma harmful? Am J Surg. 2005;190:913-7.
3. Ng JC, Swain S, Dowling JP, Wolfe R, Simpson P, Kelly JW. The impact of partial biopsy on histopathologic diagnosis of cutaneous melanoma: Experience of an Australian tertiary referral service. Arch Dermatol. 2010;146:234-9.
4. Weisberg NK, Becker DS. Potential utility of adjunctive histopathologic evaluation of some tumors treated by Mohs micrographic surgery. Dermatol Surg. 2000;26:1052-6.
5. Hennessy J, Clarke LE, Ioffreda MD, Helm KF. Enhancement of the diagnostic accuracy of large skin excision pathology reports by adding gross specimen photographs. J Cutan Pathol. 2009;36:711-2.
6. Blasdale C, Charlton FG, Weatherhead SC, Ormond P, Lawrence CM. Effect of tissue shrinkage on histological tumour-free margin after excision of basal cell carcinoma. Br J Dermatol. 2010;162:607- 10.
7. Kerns MJ, Darst MA, Olsen TG, Fenster M, Hall P, Grevey S. Shrinkage of cutaneous specimens: Formalin or other factors involved? J Cutan Pathol. 2008;35:1093-6.
8. Paterson DA, Davies JD, Mclaren KM. Failure to demonstrate the true resection margins of excised skin tumours: A case for routine marking. Br J Dermatol. 1992;127:119-21.
9. Chang TT, Somach SC, Wagamon K, Somani AK, Pomeranz J, Jaworsky C, et al. The inadequacy of punch-excised melanocytic lesions: Sampling through the block for the determination of “margins”. J Am Acad Dermatol. 2009;60:990-3.
10. Westra WH, Hruban RH, Phelps TH, Isacson C. Surgical pathology dissection: An illustrated guide. Second edition. New York: Springer; 2003.
11. Sellheyer K, Bergfeld WF. When to ask your dermatopathologist to evaluate for surgical margins and when not: A matter of confusion for dermatologists and dermatopathologists alike. J Am Acad Dermatol. 2005;52:1095-7.
12. Kolman O, Hoang MP, Piris A, Mihm MC, Duncan LM. Histologic processing and reporting of cutaneous pigmented lesions: Recommendations based on a survey of 94 dermatopathologists. J Am Acad Dermatol. 2010;63:661-7.
13. Bruecks AK, Shupe JM, Trotter MJ. Prospective step sections for small skin biopsies. Arch Pathol Lab Med. 2007;131:107-11.
14. Pickett H. Shave and punch biopsy for skin lesions. Am Fam Physician. 2011;84:995-1002.
15. Alavi A, Niakosari F, Sibbald RG. When and how to perform a biopsy on a chronic wound. Adv Skin Wound Care. 2010;23:132-40.
16. Ariza SA, Acosta A. Lentigo maligno: clínica, histopatología y tratamiento. Rev Asoc Col Dermatol. 2008;16:135-42.
17. Hazan C, Dusza SW, Delgado R, Busam KJ, Halpern AC, Nehal KS. Staged excision for lentigomaligna and lentigomaligna melanoma: A retrospective analysis of 117 cases. J Am Acad Dermatol. 2008;58:142-8.
18. Sommer LL, Barcia SM, Clarke LE, Helm KF. Persistent melanocytic nevi: A review and analysis of 205 cases. J Cutan Pathol. 2011;38:503-7.
19. Dayton AS, Ro JY, MD, Schwartz MR, Ayala AG, Raymond AK. Raymond’s paragraph system: An alternative format for the organization of gross pathology reports and its implementation in an academic teaching hospital. Arch Pathol Lab Med. 2009;133:298- 302.
20. Prieto VG, Argeny ZB, Barnhill RL, Duray PH, Elenitsas R, From L, et al. Are en face frozen sections accurate for diagnosing margin status in melanocytic lesions? Am J Clin Pathol. 2003;120:203-8.
21. Weinstein MC, Brodell RT, Bordeaux J, Honda K. The art and science of surgical margins for the dermatopathologist. Am J Dermatopathol. 2012;34:737-45.
22. Mohs FE. Chemosurgery. A microscopically controlled method of cancer excision. Arch Surg. 1941;42:279-95.
23. Trotter MJ. Melanoma margin assessment. Surgical Pathology 2009;2:543-52.
24. Scolyer RA, Judge MJ, Evans A, Frishberg DP, Prieto VG, Thompson JF, et al. Data set for pathology reporting of cutaneous invasive melanoma: Recommendations from the international collaboration on cancer reporting (ICCR). Am J Surg Pathol. 2013;37:1797- 814. Fecha de consulta: 3 de enero de 2014. Disponible en: http:// www.ncbi.nlm.nih.gov/pmc/articles/PMC3864181/.
25. Kimyai-Asadi A, Katz T, Goldberg LH, Ayala GB, Wang SQ, Vujevich JJ, et al. Margin Involvement after the excision of melanoma in situ: The need for complete en face examination of the surgical margins. Dermatol Surg. 2007;33:1434-9.
26. Kimyai-Asadi A, Alam M, Goldberg LH, Peterson SR, Silapunt S, Jih MH. Efficacy of narrow-margin excision of well-demarcated primary facial basal cell carcinomas. J Am Acad Dermatol. 2005;53:464-8.
27. Kimyai-Asadi A, Goldberg LH, Jih MH. Accuracy of serial transverse cross-sections in detecting residual basal cell carcinoma at the surgical margins of an elliptical excision specimen. J Am Acad Dermatol. 2005;53:469-74.
28. Thomas DJ, King AR, Peat BG. Excision margins for nonmelanotic skin cancer. Plast Reconstr Surg. 2003;112:57-63.
29. Clayton BD, Leshin B, Hitchcock MG, Marks M, White WL. Utility of rush paraffin-embedded tangential sections in the management of cutaneous neoplasms. Dermatol Surg. 2000;26:671-8.
30. Lichte V, Breuninger H, Metzler G, Haefner HM, Moehrle M. Acral lentiginous melanoma: Conventional histology Vs. three-dimensional histology. Br J Dermatol. 2009;160:591-9.
31. Restrepo R. Cortes transversales Vs. verticales para el diagnóstico de las alopecias. Rev Asoc Col Dermatol. 2008;16:23-8. Fecha de consulta: 1 de enero de 2014. Disponible en: http://revistasocolderma.org/files/Articulo%20de%20revision%20-%20Cortes%20 transversales%20vs%20verticales.pdf.
32. Flotte TJ. Transverse sectioning of the scalp (Headington technique) in the 19th century. J Cutan Pathol. 2008;35:82-5.
33. Bôer A, Hoene K. Transverse sections for diagnosis of alopecia? Am J Dermatopathol. 2005;27:348-52.
34. Elston DM, Ferringer T, Dalton S, Fillman E, Tyler W. A comparison of vertical versus transverse sections in the evaluation of alopecia biopsy specimens. J Am Acad Dermatol. 2005;53:267-72.
35. Bathish N, Izhak OB, Shemer A, Bergman R. A study of serial vertical sectioning of scalp biopsies to increase the histological diagnostic yield in alopecias. J Eur Acad Dermatol Venereol. 2010;24:709-15.
36. García C, Poletti E. Scalp biopsy specimens: Transverse Vs. vertical sections. Arch Dermatol. 2007;143:268.
37. Nguyen JV, Hudacek K, Whitten JA, Rubin AI, Seykora JT. The HoVert technique: A novel method for the sectioning of alopecia biopsies. J Cutan Pathol. 2011;38:401-6.
38. Shelley WB. Hair examination using double-stick tape. J Am Acad Dermatol. 1983;8:430-1.
39. Whiting DA, Dy LC. Office diagnosis of hair shaft defects. Semin Cutan Med Surg. 2006;25:24-34.
40. Zitelli JA. Pseudomonilethrix. An artifact. Arch Dermatol. 1986;122:688-90.
41. Baden HP, Kubilus J, Baden L. A stain for plucked anagen hairs. J Am Acad Dermato. 1979;1:121-2.
42. Sperling LC. Introduction to diseases of the hair. In: Demis DJ, editor. Clinical dermatology. 18th edition. New York: Lippincott; 1991. p. 1-17.
43. Caseiro RJ. Diagnostic techniques for hair disorders: III. Clinical hair manipulations and clinical findings. Cutis. 1987;40:442-8.
44. Olsen EA, Bettencourt MS, Coté NL. The presence of loose anagen hairs obtained by hair pull in the normal population. J Investig Dermatol Symp Proc. 1999;4:258-60.
45. Grover C, Nanda S, Reddy B, Chaturvedi K. Nail biopsy: Assessment of indications and outcome. Dermatol Surg. 2005;31:190-4.
46. Barrera-Vigo MV, Tejera-Vaquerizo A, Mendiola-Fernández M, Cid J, Cabra-de Luna B, Herrera-Ceballos E. Diagnostic utility of nail biopsy: A study of 15 cases. Actas Dermosifiliogr. 2008;99:621-7. Fecha de consulta: 10 de noviembre de 2013. Disponible en:http://apps.elsevier.es/watermark/ctl_servlet?_f=10&pident_ articulo=90183286&pident_usuario=0&pcontactid=&pident_re vista=403&ty=109&accion=L&origen=actasdermo&web=http:// www.actasdermo.org&lan=en&fichero=403v99n08a9018328 6pdf001.pdf.
47. Hanno R, Mathes BM, Krull EA. Longitudinal nail biopsy in evaluation of acquired nail dystrophies. J Am Acad Dermatol 1986;14:803-9.
48. deBerker DA, Dahl MG, Comaish JS, Lawrence CM. Nail surgery: An assessment of indications and outcome. Acta Derm Venereol 1996;76:484-7.
49. Rich P. Nail biopsy. Indications and methods. J Dermatol Surg Oncol. 1992;18:673-82.
50. Rich P. Nail biopsy: Indications and methods. Dermatol Surg. 2001;27:229-34.
51. Grover C, Khandpur S, Reddy B, Chaturvedi K. Longitudinal nail biopsy: Utility in 20-nail dystrophy. Dermatol Surg. 2003;29:1125-9.
52. Martin B. Nail histopathology. Actas Dermosifiliogr. 2013;104(7):564-78.
53. Haneke E. Cirugía dermatológica de la región ungular. Monogr Dermatol. 1991;6:408-11.
54. André J, Sass U, Richert B, Theunis A. Nail pathology. Clin Dermatol. 2013;31:526-39.
55. Fleckman P, Omura EF. Histopathology of the nail. Adv Dermatol. 2001;17:385-406.
56. Haneke E. Surgical anatomy of the nail apparatus. Dermatol Clin. 2006;24:291-6.
57. Weinberg JM, Koestenblatt EK, Jennings MB. Utility of histopathologic analysis in the evaluation of onychomycosis. J Am Podiatr Med Assoc 2005;95:258-63.
58. Grover C, Reddy BS, Chaturvedi KU. Onychomycosis and the diagnostic significance of nail biopsy. J Dermatol. 2003;30:116-22.
59. González-Serva A. Structure and function. In: Scher RK, DanielCR, editors. Nails: therapy, diagnosis, surgery. Philadelphia: Saunders; 1997:11-30.
60. Ruben BS. Pigmented lesions of the nail unit: Clinical and histologic features. Semin Cutan Med Surg. 2010;29:148-58.
61. Martin B. Histopatología de la uña. Actas Dermosifiliog. 2013;104:564-78.
62. Lewin K, De Wit AS, Lawson R. Softening techniques for nails biopsies. Arch Dermatol. 1973;107:223-4.
63. Piérard GE, Arrese JE, Pierre S, Bertrand C, Corcuff P, Lévêque JL, Piérard-Franchimont C. Diagnostic microscopique des onychomycoses. Ann Dermatol Venerol. 1994;121:25-9.
64. Hay RJ, Baran R, Haneke E. Fungal (onychomycosis) and other infections involving the nail apparatus. In: Baran R, Dawbern RPR, de Berker DAR, Haneke E, Tosti A, editors. Baran and Dawbern’s diseases of the nails and their management. Malden, MA: Blackwell Science; 2001:211-50.
65. Perrin C, Michiels JF, Pisani A, Ortonne JP. Anatomic distribution of melanocytes in normal nail unit: An immuno-histochemical investigation. Am J Dermatopathol. 1997;19:462-7.
66. Tosti A, Cameli N, Piraccini BM, Fanti PA, Ortonne JP. Characterization of nail matrix melanocytes with anti-PEP1, anti-PEP8, TMH-1, and HMB-45 antibodies. J Am Acad Dermatol. 1994;31:193-6.
67. Jerasutus S. Histopathology. In: Scher RK, Daniel CR 3rd, editors. Nails: Diagnosis, therapy, surgery. 3rd edition. Philadelphia: Elsevier Saunders; 2005. p. 37-70.
68. Sellheyer K, Bergfeld WF, Stewart E, Roberson G, Hammel J. Evaluation of surgical margins in melanocytic lesions: A survey among 152 dermatopathologists. J Cutan Pathol. 2005;32:293-9.
Cómo citar
Descargas
Descargas
Publicado
Cómo citar
Número
Sección

| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |






