Update of treatment of adverse cutaneous drug reactions
DOI:
https://doi.org/10.29176/2590843X.1553Keywords:
Drug hypersensitivity, Drug therapy, Skin diseasesAbstract
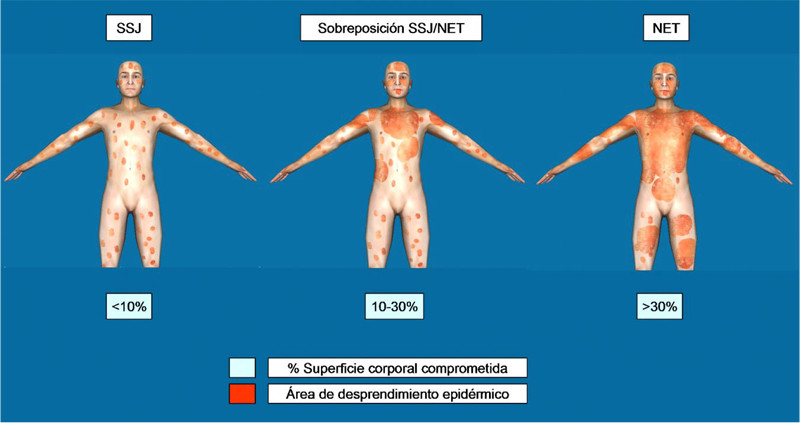
In contrast to the frequently skin eruptions related to drug reactions, the severe presentations such as drug hypersensitivity syndrome with eosinophilia and Stevens-Johnson syndrome/toxic epidermal necrolysis spectrum, can have life threatening complications. Investigations evaluating the treatment of these entities are conditioned by the critical status and the low incidence of cases, making high quality evidence limited and the most effective therapy cannot be established. This article reviews commonly applied systemic treatments in adult patients, the physiopathological substrate, therapeutic schemes and most frequent unwanted effects. Also describes new alternatives that offer potential applications.
Author Biographies
María Fernanda Meza-Corso
Médica Cirujana. Universidad Nacional de Colombia
Cesar González-Ardila
Dermatólogo. Miembro de AsoColDerma
References
2. Uetrecht J, Naisbitt DJ. Idiosyncratic adverse drug reactions: Current concepts. Pharmacol Rev. 2013;65(2):779-808. doi: 10.1124/pr.113.007450
3. González C. Reacciones medicamentosas. En: Archila P, Senior J (editores). Texto de Medicina Interna. Aprendizaje basado en problemas. Bogotá D.C.: Distribuna Editorial Médica; 2013. p. 1923-25.
4. Aihara M, Kano Y, Fujita H, Kambara T, Matsukura S, Katayama I, et al. Efficacy of additional i.v. immunoglobulin to steroid therapy in Stevens-Johnson syndrome and toxic epidermal necrolysis. J Dermatol. 2015;42(8):768-77. doi: 10.1111/1346-8138.12925
5. Kirchhof MG, Wong A, Dutz JP. Cyclosporine treatment of drug-induced hypersensitivity syndrome. JAMA Dermatol. 2016;152(11):1254-7. doi: 10.1001/jamadermatol.2016.2220
6. Wang CW, Yang LY, Chen CB, Ho HC, Hung SI, Yang CH, et al. Randomized, controlled trial of TNF-α antagonist in CTL-mediated severe cutaneous adverse reactions. J Clin Invest. 2018;128(3):985-96. doi: 10.1172/JCI93349
7. Deng Q, Fang X, Zeng Q, Lu J, Jing C, Huang J. Severe cutaneous adverse drug reactions of Chinese inpatients: A meta-analysis. An Bras Dermatol. 2017;92(3):345-9. doi: 10.1590/abd1806-4841.20175171
8. Gupta L, Martin A, Agarwal N, D’Souza P, Das S, Kumar R, et al. Guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis: An Indian perspective. Indian J Dermatol Venereol Leprol. 2016;82(6):603-25. doi: 10.4103/0378-6323.191134
9. Cabañas R, Ramírez E, Sendagorta E, Alamar R, Barranco R, Blanca-López N, et al. Spanish Guidelines for Diagnosis, Management, Treatment and Prevention of DRESS syndrome. J Investig Allergol Clin Immunol. 2020;30(4):229-253. doi: 10.18176/iiaci.0480
10. Seminario-Vidal L, Kroshinsky D, Malachowski SJ, Sun J, Markova A, Beachkofsky TM, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020;82(6):1553-67. doi: 10.1016/j.jaad.2020.02.066
11. Arias DA, Londoño PA, López JG, Moreno LH. Síndrome de Stevens-Johnson y necrolísis epidérmica tóxica en el Hospital Universitario del Valle “Evaristo García” durante un periodo de 9 años. Rev Asoc Colomb Dermatol Cir Dermatol. 2013;21(3):214-9. doi.org/10.29176/2590843X.256
12. Wu J, Lee YY, Su SC, Wu TS, Kao KC, Huang CC, et al. Stevens-Johnson syndrome and toxic epidermal necrolysis in patients with malignancies. Br J Dermatol. 2015;173(5):1224-31. doi: 10.1111/bjd.14052
13. Hirapara NH, Patel TK, Barvaliya MJ, Tripathi C. Drug-induced Stevens-Johnson Syndrome in Indian Population: A Multicentric Retrospective Analysis. Niger J Clin Pract. 2017;20(8):978-83. doi: 10.4103/njcp.njcp_122_16
14. Sotozono C, Ueta M, Nakatani E, Kitami A, Watanabe H, Sueki H, et al. Predictive Factors Associated with Acute Ocular Involvement in Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis. Am J Ophthalmol. 2015;160(2):228-237. e2. doi: 10.1016/j.ajo.2015.05.002
15. Choonhakarn C, Limpawattana P, Chaowattanapanit S. Clinical profiles and treatment outcomes of systemic corticosteroids for toxic epidermal necrolysis: A retrospective study. J Dermatol. 2016;43(2):156-61. doi: 10.1111/1346-8138.13040
16. Morita K, Matsui H, Michihata N, Fushimi K, Yasunaga H. Association of Early Systemic Corticosteroid Therapy with Mortality in Patients with Stevens-Johnson Syndrome or Toxic Epidermal Necrolysis: A Retrospective Cohort Study Using a Nationwide Claims Database. Am J Clin Dermatol. 2019;20(4):579-92. doi: 10.1007/s40257-019-00443-9
17. Middendorf MM, Busaileh AZ, Babakhani A, Marik PE. Stevens-Johnson syndrome/toxic epidermal necrolysis: Treatment with low-dose corticosteroids, Vitamin C and thiamine. BMJ Case Rep. 2019;12(11):e230538. doi: 10.1136/bcr-2019-230538
18. Funck-Brentano E, Duong TA, Bouvresse S, Bagot M, Wolkenstein P, Roujeau JC, et al. Therapeutic management of DRESS: A retrospective study of 38 cases. J Am Acad Dermatol. 2015;72(2):246-52. doi: 10.1016/j.jaad.2014.10.032
19. Allouchery M, Logerot S, Cottin J, Pralong P, Villier C, Ben Saïd B. Antituberculosis DrugAssociated DRESS: A Case Series. J Allergy Clin Immunol Pract. 2018;6(4):1373-80. doi: 10.1016/j.jaip.2017.11.021
20. Takehara A, Aoyama Y, Kurosawa M, Shirafuji Y, Umemura H, Kamiya K, et al. Longitudinal análisis of antibody profiles against plakins in severe drug eruptions: emphasis on correlation with tissue damage in drug-induced hypersensitivity síndrome and drug reaction with eosinophilia and systemic symptoms. Br J Dermatol. 2016;175(5):944-52. doi: 10.1111/bjd.14677
21. Nam YH, Park MR, Nam HJ, Lee SK, Kim KH, Roh MS, et al. Drug reaction with eosinophilia and systemic symptoms syndrome is not uncommon and shows better clinical outcome than generally recognised. Allergol Immunopathol (Madr). 2015;43(1):19-24. doi: 10.1016/j.aller.2013.08.003
22. Ocampo-Garza J, Ocampo-Garza SS, Martínez-Villarreal JD, Barbosa-Moreno LE, Guerrero-González GA, Ocampo-Candiani J. [DRESS syndrome: Report of nine cases]. Rev Med Chil. 2015;143(5):577-83. doi: 10.4067/S0034-98872015000500004
23. Díaz JC, Bonilla D, Ramírez AF, Herrera MC, Ramírez LF, Serrano CD. Grandes dosis de corticoides sistémicos en pacientes con síndrome de Stevens-Johnson y necrólisis epidérmica tóxica: descripción de siete casos y revisión de la literatura. Rev Asoc Colomb Dermatol Cir Dermatol. 2019;19(1):13-9.
24. Yamane Y, Matsukura S, Watanabe Y, Yamaguchi Y, Nakamura K, Kambara T, et al. Retrospective analysis of Stevens-Johnson síndrome and toxic epidermal necrolysis in 87 Japanese patients – Treatment and outcome. Allergol Int. 2016;65(1):74-81. doi: 10.1016/j.alit.2015.09.001
25. Zhang C, Van DN, Hieu C, Craig T. Drug-induced severe cutaneous adverse reactions: Determine the cause and prevention. Ann Allergy Asthma Immunol. 2019;123(5):483-7. doi: 10.1016/j.anai.2019.08.004
26. Shiohara T, Mizukawa Y. Drug-induced hypersensitivity syndrome (DiHS)/drug reaction with eosinophilia and systemic symptoms (DRESS): An update in 2019. Allergol Int. 2019;68(3):301-8. doi: 10.1016/j.alit.2019.03.006
27. Cardona M, Galindo LF, Díaz-Guío DA. Síndromes de hipersensibilidad inducidos por medicamentos en las unidades de cuidados intensivos. Rev Asoc Colomb Dermatol Cir Dermatol. 2018;26(3):170-83. doi: 10.29176/2590843X.58
28. Shiohara T, Kano Y, Hirahara K, Aoyama Y. Prediction and management of drug reaction with eosinophilia and systemic symptoms (DRESS). Expert Opin Drug Metab Toxicol. 2017;13(7):701-4. doi: 10.1080/17425255.2017.1297422
29. Lalosevic J, Nikolic M, Gajic-Veljic M, Skiljevic D, Medenica L. Stevens-Johnson syndrome and toxic epidermal necrolysis: A 20-year single-center experience. Int J Dermatol. 2015;54(8):978-84. doi: 10.1111/ijd.12702
30. Ye L, Zhang C, Zhu Q. The Effect of Intravenous Immunoglobulin Combined with Corticosteroid on the Progression of Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis: A MetaAnalysis. PLoS One. 2016;11(11):e0167120. doi: 10.1371/journal.pone.0167120
31. Micheletti RG, Chiesa-Fuxench Z, Noe MH, Stephen S, Aleshin M, Agarwal A, et al. Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis: A Multicenter Retrospective Study of 377 Adult Patients from the United States. J Invest Dermatol. 2018;138(11):2315-21. doi: 10.1016/j.jid.2018.04.027
32. Tran AK, Sidhu S. Stevens Johnson síndrome and toxic epidermal necrolysis–an Australian analysis of treatment outcomes and mortality. J Dermatolog Treat. 2019;30(7):718-23. doi: 10.1080/09546634.2019.1568380
33. Zimmermann S, Sekula P, Venhoff M, Motschall E, Knaus J, Schumacher M, et al. Systemic immunomodulating therapies for Stevens-Johnson syndrome and toxic epidermal necrolysis: A systematic review and metaanalysis. JAMA Dermatol. 2017;153(6):514-22. doi: 10.1001/jamadermatol.2016.5668
34. Cartotto R. Burn Center Care of Patients with Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis. Clin Plast Surg. 2017;44(3):583-95. doi: 10.1016/j.cps.2017.02.016
35. Mohanty S, Das A, Ghosh A, Sil A, Gharami R, Bandyopadhyay D, et al. Effectiveness, safety and tolerability of cyclosporine versus supportive treatment in Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis: A record-based study. Indian J Dermatol Venerol Leprol. 2017;83(3):312-6. doi: 10.4103/ijdvl.IJDVL_201_16
36. Chen YT, Hsu CY, Chien YN, Lee WR, Huang YC. Efficacy of cyclosporine for the treatment of Stevens-Johnson syndrome and toxic epidermal necrolysis: Systemic review and metaanalysis. Dermatol Sin. 2017;35(3):131-7. doi: 10.1016/j.dsi.2017.04.004
37. González-Herrada C, Rodríguez-Martín S, Cachafeiro L, Lerma V, González O, Lorente JA, et al. Cyclosporine Use in Epidermal Necrolysis Is Associated with an Important Mortality Reduction: Evidence from Three Different Approaches. J Invest Dermatol. 2017;137(10):2092-100. doi: 10.1016/j.jid.2017.05.022
38. Lee HY, Fook-Chong S, Koh HY, Thirumoorthy T, Pang SM. Cyclosporine treatment for Stevens-Johnson syndrome/toxic epidermal necrolysis: Retrospective analysis of a cohort treated in a specialized referral center. J Am Acad Dermatol. 2017;76(1):106-13. doi: 10.1016/j.jaad.2016.07.048
39. Poizeau F, Gaudin O, Le Cleach L, Duong TA, Hua C, Hotz C, et al. Cyclosporine for Epidermal Necrolysis: Absence of Beneficial Effect in a Retrospective Cohort of 174 Patients—Exposed/Unexposed and Propensity Score-Matched Analyses. J Invest Dermatol. 2018;138(6):1293-300. doi: 10.1016/j.jid.2017.12.034
40. Bastuji-Garin S, Fouchard N, Bertocchi M, Roujeau JC, Revuz J, Wolkenstein P. SCORTEN: A severity-of-illness score for toxic epidermal necrolysis. J Invest Dermatol. 2000;115(2):149-53. doi: 10.1046/j.1523-1747.2000.00061.x
41. Ng QX, De Deyn MLZQ, Venkatanarayanan N, Ho CYX, Yeo WS. A meta-analysis of cyclosporine treatment for Stevens-Johnson syndrome/toxic epidermal necrolysis. J Inflamm Res. 2018;11:135-42. doi: 10.2147/JIR.S160964
42. 42. Woolridge KF, Boler PL, Lee BD. Tumor necrosis factor α inhibitors in the treatment of toxic epidermal necrolysis. Cutis. 2018;101(1):E15-21.
43. Wolkenstein P, Latarjet J, Roujeau JC, Duguet C, Boudeau S, Vaillant L, et al. Randomised comparison of thalidomide versus placebo in toxic epidermal necrolysis. Lancet. 1998;352(9140):1586-9. doi: 10.1016/S0140-6736(98)02197-7
44. Wang R, Zhong S, Tu P, Li R, Wang M. Rapid remission of Stevens-Johnson syndrome by combination therapy using etanercept and intravenous immunoglobulin and a review of the literature. Dermatol Ther. 2019 Jul;32(4):e12832.
45. Wang F, Gao X, Chen X, Tang X, Chen H, Han J. Successful treatment of interstitial lung disease related to Stevens–Johnson syndrome/toxic epidermal necrolysis overlap with etanercept: A case report and published work review. J Dermatol. 2019;46(11):1035-8. doi: 10.1111/dth.12832
46. Pham CH, Gillenwater TJ, Nagengast E, McCullough MC, Peng DH, Garner WL. Combination therapy: Etanercept and intravenous immunoglobulin for the acute treatment of Stevens-Johnson syndrome/toxic epidermal necrolysis. Burns. 2019;45(7):1634-8. doi: 10.1016/j.burns.2018.12.018
47. Kim S, Joo EJ, Kim UJ, Kim JH, Kim B, Lee HJ, et al. Corticosteroid-induced drug reaction with eosinophilia and systematic symptoms successfully treated with a tumor necrosis factor alpha inhibitor. Asian Pac J Allergy Immunol. 2020. doi: 10.12932/AP-210819-0628.
48. Leman RE, Chen L, Shi X, Rolimpandoei SP, Ling X, Su Y. Drug reaction with eosinophilia and systemic symptoms (DRESS) successfully treated with tumor necrosis factor-α inhibitor. JAAD Case Rep. 2017;3(4):332-5. doi: 10.1016/j.jdcr.2017.05.006
49. Adil M, Amin SS, Mohtashim M. N-acetylcysteine in dermatology. Indian J Dermatol Venereol Leprol. 2018;84(6):652-9. doi: 10.4103/ijdvl.IJDVL_33_18 50. Janeczek M, Moy L, Riopelle A, Vetter O, Reserva J, Tung R, et al. The potential uses of N-acetylcysteine in dermatology: A review. J Clin Aesthet Dermatol. 2019;12(5):20-6.
51. Ichai P, Laurent-Bellue A, Saliba F, Moreau D, Besch C, Francoz C, et al. Acute Liver Failure/Injury Related to Drug Reaction With Eosinophilia and Systemic Symptoms: Outcomes and Prognostic Factors. Transplantation. 2017;101(8):1830-37. doi: 10.1097/TP.0000000000001655
52. Hsu DY, Brieva J, Silverberg NB, Silverberg JI. Morbidity and Mortality of Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis in United States Adults. J Invest Dermatol. 2016;136(7):1387-97. doi: 10.1016/j.jid.2016.03.023
53. Beck A, Cooney R, Gamelli RL, Mosier MJ. Predicting mechanical ventilation and mortality: Early and late indicators in Steven-johnson syndrome and toxic epidermal necrolysis. J Burn Care Res. 2016;37(1):e47-55. doi: 10.1097/BCR.0000000000000329
54. Lee TH, Lee CC, Ng CY, Chang MY, Chang SW, Fan PC, et al. The influence of acute kidney injury on the outcome of Stevens-Johnson syndrome and toxic epidermal necrolysis: The prognostic value of KDIGO staging. PLoS One. 2018;13(9):e0203642. doi: 10.1371/journal.pone.0203642
55. Chung WH, Chang WC, Stocker SL, Juo CG, Graham GG, Lee MHH, et al. Insights into the poor prognosis of allopurinol-induced severe cutaneous adverse reactions: The impact of renal insufficiency, high plasma levels of oxypurinol and granulysin. Ann Rheum Dis. 2015;74(12):2157-64. doi: 10.1136/annrheumdis-2014-205577
56. Bai M, Yu Y, Huang C, Liu Y, Zhou M, Li Y, et al. Continuous venovenous hemofiltration combined with hemoperfusion for toxic epidermal necrolysis: a retrospective cohort study. J Dermatolog Treat. 2017;28(4):353-9. doi: 10.1080/09546634.2016.1240326
57. Han F, Zhang J, Guo Q, Feng Y, Gao Y, Guo L, et al. Successful treatment of toxic epidermal necrolysis using plasmapheresis: A prospective observational study. J Crit Care. 2017;42:65-8. doi: 10.1016/j.jcrc.2017.07.002
58. Fathallah N, Slim R, Rached S, Hachfi W, Letaief A, Ben Salem C. Sulfasalazine-induced DRESS and severe agranulocytosis successfully treated by granulocyte colony-stimulating factor. Int J Clin Pharm. 2015;37(4):563-5. doi: 10.1007/s11096-015-0107-2
59. Thein OS, Sutton B, Thickett DR, Parekh D. Mepolizumab rescue therapy for acute pneumonitis secondary to DRESS. BMJ Case Rep. 2019;12(10):e231355. doi: 10.1136/bcr-2019-231355
60. Damsky WE, Vesely MD, Lee AI, Choi J, Meyer A-C, Chen M, et al. Drug-induced hypersensitivity syndrome with myocardial involvement treated with tofacitinib. JAAD Case Rep. 2019;5(12):1018-26. doi: 10.1016/j.jdcr.2019.07.004
61. Maximova N, Maestro A, Zanon D, Marcuzzi A. Rapid recovery of postnivolumab vemurafenibinduced Drug Rash with Eosinophilia and Systemic Symptoms (DRESS) syndrome after tocilizumab and infliximab administration. J Immunother Cancer. 2020;8(1):e000388. doi: 10.1136/jitc-2019-000388
62. Uzun R, Yalcin AD, Celik B, Bulut T, Yalcin AN. Levofloxacin induced toxic epidermal necrolysis: Successful therapy with omalizumab (antiIgE) and pulse prednisolone. Am J Case Rep. 2016;17:666-71. doi: 10.12659/ajcr.899823
63. Su SC, Mockenhaupt M, Wolkenstein P, Dunant A, Le Gouvello S, Chen CB, et al. Interleukin-15 Is Associated with Severity and Mortality in Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis. J Invest Dermatol. 2017;137(5):1065-73. doi: 10.1016/j.jid.2016.11.034
How to Cite
Downloads
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2020 Revista de la Asociación Colombiana de Dermatología y Cirugía Dermatológica

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |






