Drug eruptions: an emergency room approach
DOI:
https://doi.org/10.29176/2590843X.1728Keywords:
DRESS syndrome, Drug eruptions, Drug hypersensitivity syndrome, Drug hypersensitivity, Stevens-Johnson syndrome, Toxic epidermal necrolysisAbstract
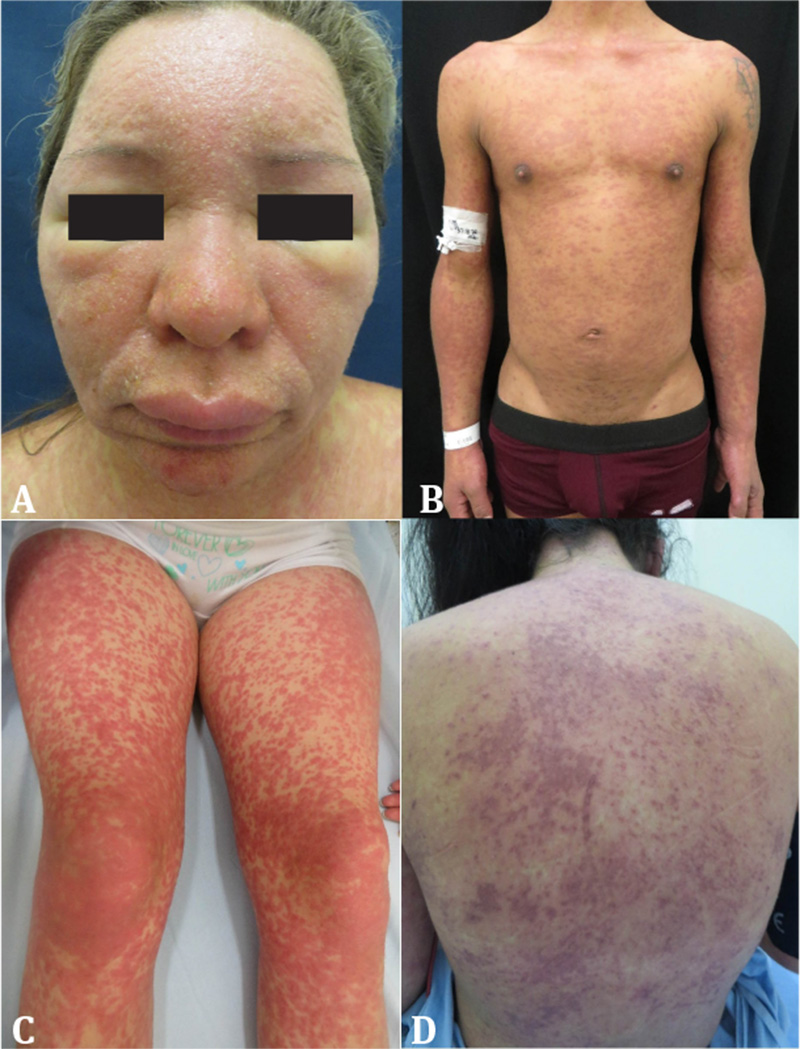
Skin eruptions are among the most common drug adverse reactions; therefore, it is usual to face them in medical practice. A systematic approach based on early identification of the possible etiologic agent, the chronology of the exposure and the clinical characteristics of the reaction, allows the clinician to categorize the severity of the disease. With a high index of suspicion, it is possible to choose the appropriate laboratory tests, to optimize medical care and take the pertinent therapeutic and preventive measures for each case. The following narrative review is intended to cover the key aspects of the most serious drug eruptions and propose a simple approach for these in the emergency department.
References
Shear N, Knowles S. Cutaneus Reactions to Drugs. En: Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell D, Wolff K (editores). Fitzpatrick’s Dermatology in General Medicine. 8.a edición. Estados Unidos: McGraw-Hill; 2012.
Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA. 1998;279(15):1200-5. https://doi.org/10.1001/jama.279.15.1200
Organización Mundial de la Salud. Formulario Modelo de la OMS 2004: Consejo general a los prescriptores: Efectos adversos e interacciones. Disponible en: https://bit.ly/3a3XuGH
Trujillo MC, Vásquez LA. Características clínicas y epidemiológicas de las toxicodermias en pacientes hospitalizados del Hospital Pablo Tobón Uribe, Medellín, Colombia, 2007-2009. Rev Asoc Colomb Dermatol. 2012;20(3):231-6. https://doi.org/10.29176/2590843X.234
Zhang J, Zixian L, Xu C, Zhao J, Kang X. Current Perspectives on Severe Drug Eruption. Clin Rev Allergy Immunol. 2021;61(3):1-17. https://doi.org/10.1007/s12016-021-08859-0
Bigby M. Rates of cutaneous reactions to drugs. Arch Dermatol. 2001;137(6):765-70.
Bolognia JL, Jorizzo JL, Schaffer JV (editores). Bolognia. Dermatología: Principales diagnósticos y tratamientos. España: Elsevier; 2015.
Khan D, Solensky R. Drug allergy. J Allergy Clin Immunol. 2010;125(2 Suppl 2):S126-137. https://doi.org/10.1016/j.jaci.2009.10.028
Romano A, Pettinato R, Andriolo M, Viola M, Guéant-Rodriguez R-M, Valluzzi RL, et al. Hypersensitivity to aromatic anticonvulsants: in vivo and in vitro cross-reactivity studies. Curr Pharm Des. 2006;12(26):3373-81. https://doi.org/10.2174/138161206778193962
Maniu C-M, Buss G, Feldmeyer L, Spertini F, Ribi C. [Severe delayed drug hypersensitivity reactions]. Rev Med Suisse. 2013;9(382):803-4, 806-11.
Celik G, Pichler WJ, Adkinson NF Jr. Drug Allergy. En: Adkinson NF, Middleton E (editores). Middleton's Allergy Principles & Practice. 7.a edi ción. Filadelfia: Mosby Elsevier; 2009. p.1205-26.
Hung SI, Chung WH, Jee SH, Chen WC, Chang YT, Lee WR, et al. Genetic susceptibility to carbamazepine-induced cutaneous adverse drug reactions. Pharmacogenet Genomics. 2006;16(4):297-306. https://doi.org/10.1097/01.fpc.0000199500.46842.4a
Dainichi T, Uchi H, Moroi Y, Furue M. StevensJohnson syndrome, drug-induced hypersensitivity syndrome and toxic epidermal necrolysis caused by allopurinol in patients with a common HLA allele: what causes the diversity? Dermatology. 2007;215(1):86-8. https://doi.org/10.1159/000102045
Tozzi V. Pharmacogenetics of antiretrovirals. Antivir Res. 2010;85(1):190-200. https://doi.org/10.1016/j.antiviral.2009.09.001
Musette P, Janela B. New Insights into Drug Reaction with Eosinophilia and Systemic Symptoms Pathophysiology. Front Med (Lausanne). 2017;4:179. https://doi.org/10.3389/fmed.2017.00179
Tempark T, Satapornpong P, Rerknimitr P, Nakkam N, Saksit N, Wattanakrai P, et al. Dapsone-induced severe cutaneous adverse drug reactions are strongly linked with HLA-B*13: 01 allele in the Thai population. Pharmacogenet Genomics. 2017;27(12):429-37. https://doi.org/10.1097/FPC.0000000000000306
McCormack M, Alfirevic A, Bourgeois S, Farrell JJ, Kasperavičiūtė D, Carrington M, et al. HLAA*3101 and carbamazepine-induced hypersensitivity reactions in Europeans. N Engl J Med. 2011;364(12):1134-43. https://doi.org/10.1056/NEJMoa1013297
Uetrecht JP. Is it possible to more accurately predict which drug candidates will cause idiosyncratic drug reactions? Curr Drug Metab. 2000;1(2):133-41. https://doi.org/10.2174/1389200003339081
Seishima M, Yamanaka S, Fujisawa T, Tohyama M, Hashimoto K. Reactivation of human herpesvirus (HHV) family members other than HHV-6 in druginduced hypersensitivity syndrome. Br J Dermatol. 2006;155(2):344-9. https://doi.org/10.1111/j.1365-2133.2006.07332.x
Ben m’rad M, Leclerc-Mercier S, Blanche P, Franck N, Rozenberg F, Fulla Y, et al. Drug-induced hypersensitivity syndrome: clinical and biologic disease patterns in 24 patients. Medicine (Baltimore). 2009;88(3):131-40. https://doi.org/10.1097/MD.0b013e3181a4d1a1
Chiou C-C, Yang L-C, Hung S-I, Chang Y-C, Kuo T-T, Ho H-C, et al. Clinicopathological features and prognosis of drug rash with eosinophilia and systemic symptoms: a study of 30 cases in Taiwan. J Eur Acad Dermatol Venereol. 2008;22(9):1044-9. https://doi.org/10.1111/j.1468-3083.2008.02585.x
Ding WY, Lee CK, Choon SE. Cutaneous adverse drug reactions seen in a tertiary hospital in Johor, Malaysia. Int J Dermatol. 2010;49(7):834-42. https://doi.org/10.1111/j.1365-4632.2010.04481.x
Häusermann P, Harr T, Bircher AJ. Baboon syndrome resulting from systemic drugs: is there strife between SDRIFE and allergic contact dermatitis syndrome? Contact Dermatitis. 2004;51(5-6):297-310. https://doi.org/10.1111/j.0105-1873.2004.00445.x
Swanson L, Colven RM. Approach to the Patient with a Suspected Cutaneous Adverse Drug Reaction. Med Clin North Am. 2015;99(6):1337-48. https://doi.org/10.1016/j.mcna.2015.06.003
Inamadar AC, Palit A. Acute skin failure: concept, causes, consequences and care. Indian J Dermatol Venereol Leprol. 2005;71(6):379-85. https://doi.org/10.4103/0378-6323.18007
Merritt HH, Putnam TJ. Sodium diphenyl hydantoinate in the treatment of convulsive disorders. J Am Med Assoc. 1938;111(12):1068-73.
Bocquet H, Bagot M, Roujeau JC. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (Drug Rash with Eosinophilia and Systemic Symptoms: DRESS). Semin Cutan Med Surg. 1996;15(4):250-7. https://doi.org/10.1016/s1085-5629(96)80038-1
Husain Z, Reddy BY, Schwartz RA. DRESS syn drome: Part I. Clinical perspectives. J Am Acad Dermatol. 2013;68(5):693.e1-14; quiz 706-8. https://doi.org/10.1016/j.jaad.2013.01.033
Muller P, Dubreil P, Mahé A, Lamaury I, Salzer B, Deloumeaux J, et al. Drug Hypersensitivity Syndrome in a West-Indian population. Eur J Dermatol. 2003;13(5):478-81.
Shiohara T, Kano Y. Drug reaction with eosinophilia and systemic symptoms (DRESS): incidence, pathogenesis and management. Expert Opin Drug Saf. 2017;16(2):139-47. https://doi.org/10.1080/14740338.2017.1270940
Tennis P, Stern RS. Risk of serious cutaneous disorders after initiation of use of phenytoin, carbamazepine, or sodium valproate: a record linkage study. Neurology. 1997;49(2):542-6. https://doi.org/10.1212/wnl.49.2.542
Guberman AH, Besag FM, Brodie MJ, Dooley JM, Duchowny MS, Pellock JM, et al. Lamotrigine associated rash: risk/benefit considerations in adults and children. Epilepsia. 1999;40(7):985-91. https://doi.org/10.1111/j.1528-1157.1999.tb00807.x
Kim GY, Anderson KR, Davis DMR, Hand J, Tollefson M. Drug reaction with eosinophilia and systemic symptoms (DRESS) in the pediatric population: A systematic review of the literature. J Am Acad Dermatol. 2020;83(5):1323-30. https://doi.org/10.1016/j.jaad.2020.03.081
Mattoussi N, Mansour AB, Essadam L, Guedri R, Fitouri Z, Becher S. Drug Reaction With Eosinophilia and Systemic Symptoms (DRESS) Syndrome in Children: A Case Report. J Investig Allergol Clin Immunol. 2017;27(2):144-6. https://doi.org/10.18176/jiaci.0140
Cacoub P, Musette P, Descamps V, Meyer O, Speirs C, Finzi L, et al. The DRESS syndrome: a literature review. Am J Med. 2011;124(7):588-97. https://doi.org/10.1016/j.amjmed.2011.01.017
Kardaun SH, Sekula P, Valeyrie-Allanore L, Liss Y, Chu CY, Creamer D, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS): an original multisystem adverse drug reaction. Results from the prospective RegiSCAR study. Br J Dermatol. 2013;169(5):1071-80. https://doi.org/10.1111/bjd.12501
Kardaun SH, Sidoroff A, Valeyrie-Allanore L, Halevy S, Davidovici BB, Mockenhaupt M, et al. Variability in the clinical pattern of cutaneous side effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br J Dermatol. 2007;156(3):609-11. https://doi.org/10.1111/j.1365-2133.2006.07704.x
Ichai P, Laurent-Bellue A, Saliba F, Moreau D, Besch C, Francoz C, et al. Acute Liver Failure/Injury Related to Drug Reaction With Eosinophilia and Systemic Symptoms: Outcomes and Prognostic Factors. Transplantation. 2017;101(8):1830-7. https://doi.org/10.1097/TP.0000000000001655
Walsh S, Creamer D. Drug reaction with eosinophilia and systemic symptoms (DRESS): a clinical update and review of current thinking. Clin Exp Dermatol. 2011;36(1):6-11. https://doi.org/10.1111/j.1365-2230.2010.03967.x
Tetart F, Picard D, Janela B, Joly P, Musette P. Prolonged evolution of drug reaction with eosinophilia and systemic symptoms: clinical, virologic, and biological features. JAMA Dermatol. 2014;150(2):206-7. https://doi.org/10.1001/jamadermatol.2013.6698
Kano Y, Shiohara T. The variable clinical picture of drug-induced hypersensitivity syndrome/drug rash with eosinophilia and systemic symptoms in relation to the eliciting drug. Immunol Allergy Clin North Am. 2009;29(3):481-501. https://doi.org/10.1016/j.iac.2009.04.007
Valeyrie-Allanore L, Sassolas B, Roujeau J-C. Drug-induced skin, nail and hair disorders. Drug Saf. 2007;30(11):1011-30. https://doi.org/10.2165/00002018-200730110-00003
Bachot N, Roujeau J-C. Differential diagnosis of severe cutaneous drug eruptions. Am J Clin Dermatol. 2003;4(8):561-72. https://doi.org/10.2165/00128071-200304080-00006
Schnyder B, Pichler WJ. Mechanisms of Drug-Induced Allergy. Mayo Clin Proc. 2009;84(3):268-72. https://doi.org/10.1016/S0025-6196(11)61145-2
Uhara H, Saiki M, Kawachi S, Ashida A, Oguchi S, Okuyama R. Clinical course of drug-induced hypersensitivity syndrome treated without systemic corticosteroids. J Eur Acad Dermatol Venereol. 2013;27(6):722-6. https://doi.org/10.1111/j.1468-3083.2012.04547.x
Funck-Brentano E, Duong T-A, Bouvresse S, Bagot M, Wolkenstein P, Roujeau J-C, et al. Therapeutic management of DRESS: a retrospective study of 38 cases. J Am Acad Dermatol. 2015;72(2):246-52. https://doi.org/10.1016/j.jaad.2014.10.032
Zuliani E, Zwahlen H, Gilliet F, Marone C. Vancomycin-induced hypersensitivity reaction with acute renal failure: resolution following cyclosporine treatment. Clin Nephrol. 2005;64(2):155-8. https://doi.org/10.5414/cnp64155
Kirchhof MG, Wong A, Dutz JP. Cyclosporine Treatment of Drug-Induced Hypersensitivity Syndrome. JAMA Dermatol. 2016;152(11):1254-7. https://doi.org/10.1001/jamadermatol.2016.2220
Ushigome Y, Kano Y, Ishida T, Hirahara K, Shiohara T. Short- and long-term outcomes of 34 patients with drug-induced hypersensitivity syndrome in a single institution. J Am Acad Dermatol. 2013;68(5):721-8. https://doi.org/10.1016/j.jaad.2012.10.017
Stevens AM, Johnson FC. A new eruptive fever associated with stomatitis and ophthalmia: report of two cases in children. Am J Dis Child. 1922;24(6):526-33. https://doi.org/10.1001/archpedi.1922.04120120077005
Lyell A. Toxic epidermal necrolysis: an eruption resembling scalding of the skin. Br J Dermatol. 1956;68(11):355-61. https://doi.org/10.1111/j.1365-2133.1956.tb12766.x
Stern RS, Divito SJ. Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis: Associations, Outcomes, and Pathobiology-Thirty Years of Progress but Still Much to Be Done. J Invest Dermatol. 2017;137(5):1004-8. https://doi.org/10.1016/j.jid.2017.01.003
Paquet P, Piérard GE. New Insights in Toxic Epidermal Necrolysis ( Lyeirs Syndrome): clinical considerations, pathobiology and targeted treatments revisited. Drug Saf. 2010;33(3):189-212. https://doi.org/10.2165/11532540-000000000-00000
Rzany B, Mockenhaupt M, Baur S, Schröder W, Stocker U, Mueller J, et al. Epidemiology of erythema exsudativum multiforme majus, Stevens-Johnson syndrome, and toxic epidermal necrolysis in Germany (1990-1992): structure and results of a population-based registry. J Clin Epidemiol. 1996;49(7):769-73. https://doi.org/10.1016/0895-4356(96)00035-2
Sekula P, Dunant A, Mockenhaupt M, Naldi L, Bouwes Bavinck JN, Halevy S, et al. Comprehensive survival analysis of a cohort of patients with Stevens-Johnson syndrome and toxic epidermal necrolysis. J Invest Dermatol. 2013;133(5):1197-204. https://doi.org/10.1038/jid.2012.510
Correia O, Delgado L, Ramos JP, Resende C, Torrinha JA. Cutaneous T-cell recruitment in toxic epidermal necrolysis. Further evidence of CD8+ lymphocyte involvement. Arch Dermatol. 1993;129(4):466-8.
Nassif A, Bensussan A, Boumsell L, Deniaud A, Moslehi H, Wolkenstein P, et al. Toxic epidermal necrolysis: effector cells are drug-specific cytotoxic T cells. J Allergy Clin Immunol. 2004;114(5):1209-15. https://doi.org/10.1016/j.jaci.2004.07.047
Wei C-Y, Chung W-H, Huang H-W, Chen Y-T, Hung S-I. Direct interaction between HLA-B and carbamazepine activates T cells in patients with Stevens-Johnson syndrome. J Allergy Clin Immunol. 2012;129(6):1562-1569.e5. https://doi.org/10.1016/j.jaci.2011.12.990
Roujeau J-C, Bricard G, Nicolas J-F. Drug-induced epidermal necrolysis: Important new piece to end the puzzle. J Allergy Clin Immunol. 2011;128(6):1277-8. https://doi.org/10.1016/j.jaci.2011.10.015
Ko T-M, Chung W-H, Wei C-Y, Shih H-Y, Chen J-K, Lin C-H, et al. Shared and restricted T-cell receptor use is crucial for carbamazepine-induced Stevens-Johnson syndrome. J Allergy Clin Immunol. 2011;128(6):1266-76.e11. https://doi.org/10.1016/j.jaci.2011.08.013
Yoshioka M, Sawada Y, Nakamura M. Diagnostic Tools and Biomarkers for Severe Drug Eruptions. Int J Mol Sci. 2021;22(14):7527. https://doi.org/10.3390/ijms22147527
Chung W-H, Hung S-I, Yang J-Y, Su S-C, Huang S-P, Wei C-Y, et al. Granulysin is a key mediator for disseminated keratinocyte death in Stevens-Johnson syndrome and toxic epidermal necrolysis. Nat Med. 2008;14(12):1343-50. https://doi.org/10.1038/nm.1884
Mittmann N, Knowles SR, Koo M, Shear NH, Rachlis A, Rourke SB. Incidence of toxic epidermal necrolysis and Stevens-Johnson Syndrome in an HIV cohort: an observational, retrospective case series study. Am J Clin Dermatol. 2012;13(1):49-54. https://doi.org/10.2165/11593240-000000000-00000
Gillis NK, Hicks JK, Bell GC, Daly AJ, Kanetsky PA, McLeod HL. Incidence and Triggers of Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis in a Large Cancer Patient Cohort. J Invest Dermatol. 2017;137(9):2021-3. https://doi.org/10.1016/j.jid.2017.05.010
Sassolas B, Haddad C, Mockenhaupt M, Dunant A, Liss Y, Bork K, et al. ALDEN, an algorithm for assessment of drug causality in Stevens-Johnson Syndrome and toxic epidermal necrolysis: comparison with case-control analysis. Clin Pharmacol Ther. 2010;88(1):60-8. https://doi.org/10.1038/clpt.2009.252
Mockenhaupt M, Viboud C, Dunant A, Naldi L, Halevy S, Bouwes Bavinck J, et al. Stevens-Johnson syndrome and toxic epidermal necrolysis: assessment of medication risks with emphasis on recently marketed drugs. The EuroSCAR-study. J Invest Dermatol. 2008;128(1):35-44. https://doi.org/10.1038/sj.jid.5701033
Harr T, French LE. Toxic epidermal necrolysis and Stevens-Johnson syndrome. Orphanet J Rare Dis. 2010;5(1):39. https://doi.org/10.1186/1750-1172-5-39
Bastuji-Garin S, Fouchard N, Bertocchi M, Roujeau JC, Revuz J, Wolkenstein P. SCORTEN: a severity of-illness score for toxic epidermal necrolysis. J Invest Dermatol. 2000;115(2):149-53. https://doi.org/10.1046/j.1523-1747.2000.00061.x
Guégan S, Bastuji-Garin S, Poszepczynska-Guigné E, Roujeau J-C, Revuz J. Performance of the SCORTEN during the first five days of hospitalization to predict the prognosis of epidermal necrolysis. J Invest Dermatol. 2006;126(2):272-6. https://doi.org/10.1038/sj.jid.5700068
Cartotto R, Mayich M, Nickerson D, Gomez M. SCORTEN accurately predicts mortality among toxic epidermal necrolysis patients treated in a burn center. J Burn Care Res. 2014;29(1):141-6. https://doi.org/10.1097/BCR.0b013e31815f3865
Trent JT, Kirsner RS, Romanelli P, Kerdel FA. Use of SCORTEN to accurately predict mortality in patients with toxic epidermal necrolysis in the United States. Arch Dermatol. 2004;140(7):890-2. https://doi.org/10.1001/archderm.140.7.890
Garg T, Sanke S, Ahmed R, Chander R, Basu S. Stevens-Johnson syndrome and toxic epidermal necrolysis-like cutaneous presentation of chikungunya fever: A case series. Pediatr Dermatol. 2018;35(3):392-6. https://doi.org/10.1111/pde.13450
Dorafshar AH, Dickie SR, Cohn AB, Aycock JK, O’Connor A, Tung A, et al. Antishear therapy for toxic epidermal necrolysis: an alternative treatment approach. Plast Reconstr Surg. 2008;122(1):154-60. https://doi.org/10.1097/PRS.0b013e3181773d5d
Ng QX, De Deyn MLZQ, Venkatanarayanan N, Ho CYX, Yeo W-S. A meta-analysis of cyclosporine treatment for Stevens-Johnson syndrome/toxic epidermal necrolysis. J Inflamm Res. 2018;11:135-42. https://doi.org/10.2147/JIR.S160964
Zimmermann S, Sekula P, Venhoff M, Motschall E, Knaus J, Schumacher M, et al. Systemic Immunomodulating Therapies for Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis: A Systematic Review and Meta-analysis. JAMA Dermatol. 2017;153(6):514-22. https://doi.org/10.1001/jamadermatol.2016.5668
Mockenhaupt M. The current understanding of Stevens-Johnson syndrome and toxic epidermal necrolysis. Expert Rev Clin Immunol. 2011;7(6):803-13; quiz 814-5. https://doi.org/10.1586/eci.11.66
Finkelstein Y, Soon GS, Acuna P, George M, Pope E, Ito S, et al. Recurrence and outcomes of Stevens-Johnson syndrome and toxic epidermal necrolysis in children. Pediatrics. 2011;128(4):723-8. https://doi.org/10.1542/peds.2010-3322
Schwartz R, McDonough PH, Lee BW. Toxic epidermal necrolysis: Part II. Prognosis, sequelae, diagnosis, differential diagnosis, prevention, and treatment. J Am Acad Dermatol. 2013;69(2):187. e1-16; quiz 203-4. https://doi.org/10.1016/j.jaad.2013.05.002
Yip LW, Thong BY, Lim J, Tan a W, Wong HB, Handa S, et al. Ocular manifestations and complications of Stevens-Johnson syndrome and toxic epidermal necrolysis: an Asian series. Allergy. 2007;62(5):527-31. https://doi.org/10.1111/j.1398-9995.2006.01295.x
Meneux E, Wolkenstein P, Haddad B, Roujeau JC, Revuz J, Paniel BJ. Vulvovaginal involvement in toxic epidermal necrolysis: a retrospective study of 40 cases. Obstet Gynecol. 1998;91(2):283-7. https://doi.org/10.1016/s0029-7844(97)00596-6
Sheridan RL, Schulz JT, Ryan CM, Schnitzer JJ, Lawlor D, Driscoll DN, et al. Long-Term Consequences of Toxic Epidermal Necrolysis in Children. Pediatrics. 2002;109(1):74-8. https://doi.org/10.1542/peds.109.1.74
Atzori L, Perla S, Atzori MG, Ferreli C, Rongioletti F. Cutaneous drug eruptions associated with COVID-19 therapy. JAAD Int. 2020;1(1):73-6. https://doi.org/10.1016/j.jdin.2020.05.004
Ramirez E, Urroz M, Rodríguez A, González-Muñoz M, Martín-Vega A, Villánet Y, et al. Incidence of Suspected Serious Adverse Drug Reactions in Corona Virus Disease-19 Patients Detected by a Pharmacovigilance Program by Laboratory Signals in a Tertiary Hospital in Spain: Cautionary Data. Front Pharmacol. 2020 ;11:602841. https://doi.org/10.3389/fphar.2020.602841
How to Cite
Downloads
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Revista de la Asociación Colombiana de Dermatología y Cirugía Dermatológica

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |






