Staphylococcus aureus: sensitivity and resistance to antibiotics in a sample of patients with atopic dermatitis. Bogota, Colombia
Keywords:
atopic dermatitis, Staphylococcus aureus, anti-bacterial agentsAbstract
Introduction: Staphylococcus aureus is present in 90% of patients with atopic dermatitis, being a factor for frequent exacerbations of the disisease.
Objetives: To determine the frequency of Staphylococcus aureus (SA) in skin lesions of patients with atopic dermatitis and their caregivers, measuring the sensitivity and resistance to conventional antibiotics.
Methodology: This is a descriptive study with a sample of 100 patients and their caregivers. We cultured skin lesions of the patients and nasal reservoirs of their caregivers in the period between May and July of 2009.
Results: We recruited 46 girls and 54 children with their caregivers. In total 56 positive cultures were obtained with SA, 23 children and 33 caregivers, and of these, 9 were concordant between caregiver and the patient. 3 cultures were methicillin resistant SA (MRSA). 51 cultures were resistant to cephalexin (91%), 56 resistant to cefadroxil (100%), 2 resistant to oxacillin (3.5%), 1 resistant to clindamycin (1.7%), 1 gentamicin-resistant (1.7%), 2 resistant to mupirocin (3.5%), and none was resistant to trimetrhopim-sulfamethoxazole or to fusidic acid.
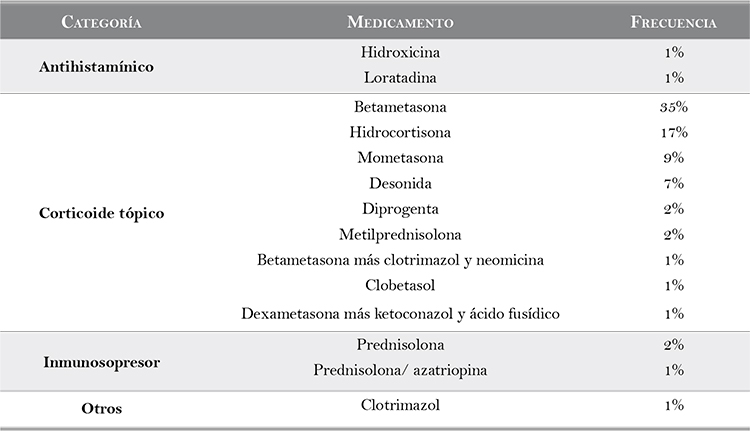
Discussion: We consider a possible association between caregiver and patient as colonists for patients with SA. There is good general susceptibility profile, but calls the attention the high resistance to cephalosporins and not to penicillinase, suggesting a possible induction of resistance given the high frequency in cephalosporins use. The topical antibiotics in reservoirs generally show a good sensitivity to S. aureus, including against MRSA. Noteworthy is the presence of the in the general population (1.5% in our study) that makes us alert to its acquisition in the community.
Author Biographies
Manuel Darío Franco
Dermatólogo, Universidad El Bosque, Bogotá, Colombia
Adriana Motta
Dermatóloga. Directora del posgrado de dermatología, Universidad El Bosque. Directora del departamento de dermatología, Hospital Simón Bolívar, Bogotá, Colombia.
Natalia Mendoza
Dermatóloga, Universidad Javeriana. Maestría en bioestadística clínica, Universidad Javeriana, Bogotá, Colombia.
References
2. García-Rodríguez JA, Gutiérrez N, Muñoz J. Ácido fusídico. Rev Esp Quimioterap. 2003;16:161-71.
3. Dobie D, Gray J. Fusidic acid resistance in Staphylococcus aureus. Arch Dis Child. 2004;89:74-7.
4. Mason B, Howard A, Magee J. Fusidic acid resistance in a community isolates of methicillin-susceptible Staphylococcus aureus and fusidic acid prescribing. J Antimicrob Chemother. 2003;51:1033-6.
5. Arkwright P, Titilayo D, Debasis S, Tinothy D, Patel L. Agerelated prevalence and antibiotic resistance of pathogenic Staphylococci and Streptococci in children with infected atopic dermatitis at a single-speciality center. Arch Dermatol. 2002;138:939-41.
6. Poyner TF, Dass BD. Comparative efficacy and tolerability of fusidic acid/hydrocortisone cream (Fucidin H cream) and miconazole/hydrocortisone cream (Daktacort cream) in the infected eczema. J Eur Acad Dermatol Venereol. 1996;7(Suppl.1):S23-30.
7. Martineau F, Picard FJ, Lansac N, Menard C, Roy PH, Oullette M, Berteron M. Correlation between the resistance genotype determined by multiplex PCR assays and the antibiotic susceptibility patterns of Staphylococcus aureus and Staphylococcus epidermidis. Antimicrobial Agents and Chemotherapy. 2000;44:231-8.
8. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing: M7-A7. Wayne, PA: Clinical and Laboratory Standards Institute; 2006.
9. Clinical and Laboratory Standards Institute. (2006). Performance standards for antimicrobial Disk susceptibility tests: M2-A9. Wayne, PA: Clinical and Laboratory Standards Institute; 2006.
10. Ramsay C, Savoie JM, Gilbert M, Gidon M, Paul K. The treatment of atopic dermatitis with topical fusidic acid and hydrocortisone acetate. J Eur Acad Dermatol Venereol. 1996;7(Suppl.1):S15-22.
11. Cardona ID, Cho SH, Leyng DY. role of bacterial superantigens in atopic dermatitis. Am J Clin Dermatol. 2006;7:273-9.
12. Boguniewicz M, Leung DYM. Atopic dermatitis. J Allergy Clin Immunol. 2006;117:S475-9.
13. Kluytmans J, van Belkum A, Verbrugh H. Nasal carriage of Staphylococcus aureus: Epidemiology, underlying mechanisms, and associated risks. Clin Microbiol Rev. 1997;10:505-20.
How to Cite
Downloads
Downloads
Published
How to Cite
Issue
Section
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |






