Ultrasonido de alta resolución en enfermedades benignas de la piel
DOI:
https://doi.org/10.29176/2590843X.124Palabras clave:
ultrasonido de alta resolución, pilomatrixoma, dermoide, hidradenitis supurativa, paniculitis, quisteResumen
La Dermatología es una rama de la Medicina en la que se ha sentido ampliamente el impacto del desarrollo tecnológico del ultrasonido de alta resolución. En la actualidad, son múltiples sus indicaciones tanto en enfermedades benignas como malignas, y siguen creciendo día a día en beneficio de los pacientes.
El ultrasonido no pretende reemplazar la juiciosa interpretación clínica del dermatólogo ni otras herramientas disponibles, como la dermatoscopia. Por el contrario, es una herramienta adicional que brinda información útil, invisible al ojo clínico, y que confirma, descarta o apoya el diagnóstico del médico tratante. El ultrasonido de alta resolución es preciso, accesible y de bajo costo, en comparación con otros métodos diagnósticos.
En este artículo se revisan sus indicaciones, hallazgos y ventajas en algunas de las enfermedades dermatológicas benignas más frecuentes.
Biografía del autor/a
Claudia Patricia González, IDIME, Bogotá, D.C., Colombia
Médica radióloga, especialista en Ecografía Dermatológica y Músculo-esquelética, IDIME, Bogotá, D.C., Colombia
Referencias bibliográficas
Wortsman X. Common applications of dermatologic sonography. J Ultrasound Med. 2012;31:97-111. https://doi.org/10.7863/jum.2012.31.1.97
González CP. Ultrasound of dermatologic lesions. Rev Colomb Radiol. 2014;25:4006-14.
Worstman X. Sonography of dermatologic emergencies. J Ultrasound Med. 2017;36:1905-14. https://doi.org/10.1002/jum.14211
Worstman X, Alfagame F, Roustan G, Arias-Santiago S, Martorell A, Catalano O, et al. Guidelines for performing dermatologic ultrasound examinations by the DERMUS group. J Ultrasound Med. 2016;35:e111-4. https://doi.org/10.7863/ultra.15.06046
Ahuja F, Quiasúa C, Martínez H, González C. Nail unit ultrasound: Applications in dermatological practice. Rev Asoc Colomb Dermatol. 2016;24:290-6.
Polanzka A, Dańczak-Pazdrowska A, Jałowska M, Żaba R, Adamski Z. Current applications of high-frequency ultrasonography in dermatology. Dermatol Alergol. 2017;34:535-42. doi: 10.5114/ada.2017.72457. https://doi.org/10.5114/ada.2017.72457
Wortsman X. Ultrasound in dermatology: why, how and when? Semin Ultrasound CT MR. 2013;34:177-95. https://doi.org/10.1053/j.sult.2012.10.001
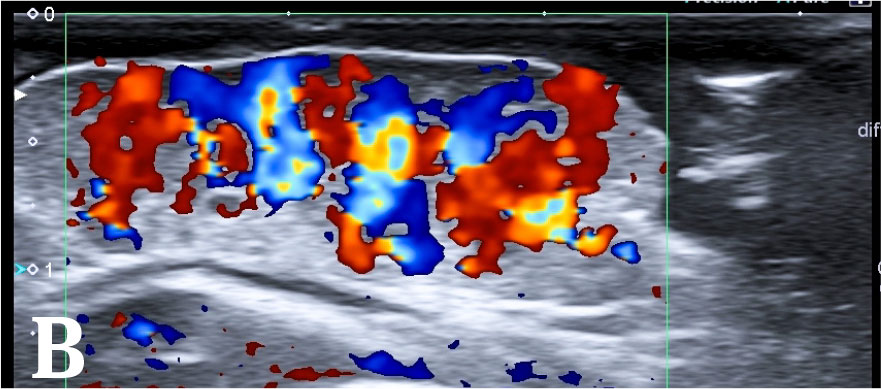
Gaitini D. Introduction to color Doppler ultrasound of the skin. En: Wortsman X, Jemec GBE, editors. Dermatologic ultrasound with clinical and histologic correlation.New York: SpringerVerlag; 2013. p. 3-14. https://doi.org/10.1007/978-1-4614-7184-4_1
Giovagnorio F, Valentini C, Paonesssa A. Highresolution and color Doppler sonography in the evaluation of skin metastases. J Ultrasound Med. 2003;22:1017-25 https://doi.org/10.7863/jum.2003.22.10.1017
Cammarota T, Pinto F, Magliario A, Sarno A. Current uses of diagnostic high-frequency US in dermatology. Eur J Radiol. 1998;27(Suppl.2):S215-23. https://doi.org/10.1016/S0720-048X(98)00065-5
Bobadilla F, Wortsman X, Muñoz C, Segovia L, Espinoza M, Jemec GB. Pre-surgical high-resolution ultrasound of facial basal cell carcinoma: Correlation with histology. Cancer Imaging. 2008;8:163-72. https://doi.org/10.1102/1470-7330.2008.0026
Wortsman X. Sonography of facial cutaneous basal cell carcinoma: A first-line imaging technique. J Ultrasound Med. 2013;32:567-72. https://doi.org/10.7863/jum.2013.32.4.567
Wortsman X, Vergara P, Castro A, Saavedra D, Bobadilla F, Sazunic I, et al. Ultrasound as predictor of histologic subtypes linked to recurrence in basal cell carcinoma of the skin. J Eur Acad Dermatol Venereol. 2015;29:702-7. https://doi.org/10.1111/jdv.12660
Schmid-Bendtner MH, Burgdorf W. Ultrasound scanning in dermatology. Arch Dermatol. 2005;141:217-24. https://doi.org/10.1001/archderm.141.2.217
Restrepo R, Palani R, Cervantes LF, Duarte AM, Amjad I, Altman NR.Hemangiomas revisited: The useful, the unusual and the new. Part 1. Overview and clinical and imaging characteristics. Pediatr Radiol. 2011;41:895-904. https://doi.org/10.1007/s00247-011-2076-5
Restrepo R, Palani R, Cervantes LF, Duarte AM, Amjad I, Altman NR. Hemangiomas revisited: The useful, the unusual and the new. Part 2. Endangering hemangiomas and treatment. Pediatr Radiol. 2011;41:905-15. https://doi.org/10.1007/s00247-011-2090-7
Restrepo R. Multimodality imaging of vascular anomalies. Pediatr Radiol. 2013;43:141-54 https://doi.org/10.1007/s00247-012-2584-y
Redondo P. Vascular malformations. (I). Concept, classifications, pathogenesis and clinical features. Actas Dermasifiliogr. 2007;98:141-58. https://doi.org/10.1016/S1578-2190(07)70418-3
White CL, Olivieri B, Restrepo R, Mckeon B, Karakas So, Lee EY. Low-flow vascular malformations pitfalls: From clinical examination to practical imaging evaluations. Part 1. Lymphatic malformations mimickers. AJR. 2016;206:940-51. https://doi.org/10.2214/AJR.15.15793
Mittal MK, Malik A, Sureka B, Thukral BB. Cystic masses of neck: A pictorial review. Indian J Radiol Imaging. 2012;22:33443. doi: 10.4103/0971-3026.111488 https://doi.org/10.4103/0971-3026.111488
Ahuja AT, King AD, Metreweli C. Second brachial cleft cysts: Variability of sonographic appearances in adult cases. AJNR AM J Neuroradiol. 2000;21:315-9.
Narayana-Moorthy S, Arcot R. Thyroglossal duct cyst-More than just an embryological remnant. Indian J Surg. 2011;73:28-31. https://doi.org/10.1007/s12262-010-0171-8
Smirniotopous JG, Chiechi MV. Teratomas, dermoid, and epidermoids of head and neck. Radiographics. 1995;15:1437-55. https://doi.org/10.1148/radiographics.15.6.8577967
Rippey JC, Royse AG. Ultrasound in trauma. Best Pract Res Clin Anaesthesiol. 2009;23:343-62. https://doi.org/10.1016/j.bpa.2009.02.011
Mankad K, Hoey E, Grainger AJ, Barron DA. Trauma musculoskeletal ultrasound. Emerg Radiol. 2008;15:83-9. doi: 10.1007/s10140-007-0691-0. https://doi.org/10.1007/s10140-007-0691-0
Draghi F, Zacchino M, Canepari M, Nucci P, Alessandrino F. Muscle injuries: Ultrasound evaluation in the acute phase. J Ultrasound. 2013;16:209-14. doi: 10.1007/s40477-013-0019-8 https://doi.org/10.1007/s40477-013-0019-8
Neal C, Jacobson JA, Brandon C, Kalume-Brigido M, Morag Y, Girish G. Sonography of Morel-Lavallée lesions. J Ultrasound Med. 2008;27:1077-81. https://doi.org/10.7863/jum.2008.27.7.1077
Spain JA, Rheinboldt M, Parrish D, Rinker E. Morel-Lavallée injuries: A multimodality approach to imaging characteristics. Acad Radiol. 2017;24:220-5. doi: 10.1016/j.acra.2016.08.029 https://doi.org/10.1016/j.acra.2016.08.029
Horton LK, Jacobson J, Powell A, Fessell D, Curtis W. Hayes sonography and radiography of softtissue foreign bodies. AJR. 2001;176:1155-9. https://doi.org/10.2214/ajr.176.5.1761155
Jarraya M, Hayashi D, Villiers R, Roemer FW, Murakami AM, Cossi A, et al. Multimodality imaging of foreign bodies of the musculoskeletal system. AJR. 2014;203:W92-102. 10.2214/AJR.13.11743 https://doi.org/10.2214/AJR.13.11743
Jacobson JA, Powell A, Craig JG, Bouffard JA, van Holsbeeck MT. Wooden foreign bodies in soft tissue: Detection at US. Radiology. 1998;206:45-8. https://doi.org/10.1148/radiology.206.1.9423650
Shiels WE, Babcock DS, Wilson JL, Burch RA. Localization and guided removal of soft-tissue foreign bodies with sonography. AJR. 1990;155:1277-81. https://doi.org/10.2214/ajr.155.6.2122680
Wortsman X. Inflammatory diseases of the skin. En: Wortsman X, Jemec GBE, editors. Dermatologic ultrasound with clinical and histologic correlation. New York: Springer; 2013. p. 73-118. https://doi.org/10.1007/978-1-4614-7184-4_4
Naouri M, Samimi M, Atlan M, Perrideau E, Vallin C, Zakine G et al. High-resolution cutaneous ultrasonography to differentiate lipoedema from lymphoedema. Br J Dermatol. 2010;163:296-301. https://doi.org/10.1111/j.1365-2133.2010.09810.x
Chen LF, Lu CH, Shen CY, Hsieh SC, Li KJ. Sonographic findings of cutaneous panniculitis in systemic lupus erythematosus and/or antiphospholipid syndrome: A case series. Ultrasound Med Biol. 2017;43:S196-7. https://doi.org/10.1016/j.ultrasmedbio.2017.08.1670
Kurayev A, Ashkar H, Saraiya A, Gottlieb AB. Hidradenitis suppurativa: Review of the pathogenesis and treatment. J Drugs Dermatol. 2016;15:1017-22.
von der Werth JM, Williams HC. The natural history of hidradenitis suppurativa. J Eur Acad Dermatol Venereol. 2000;14:389-92. https://doi.org/10.1046/j.1468-3083.2000.00087.x
Worstman X. Imaging of hidradenitis suppurativa. Dermatol Clin. 2016;34:59-68. https://doi.org/10.1016/j.det.2015.08.003
Martorell A, Segura JM. Ultrasound examination of hidradenitis suppurativa. Actas Dermosifiliogr. 2015;106(Suppl.1):49-59. https://doi.org/10.1016/S0001-7310(16)30007-2
Wortsman X, Rodríguez C, Lobos C, Eguiguren G. Ultrasound diagnosis and staging in pediatric hidradenitis suppurativa. Pediatr Dermatol. 2016;33:e260-4. doi: 10.1111/pde.12895 https://doi.org/10.1111/pde.12895
Wortsman X, Jemec GBE. A 3D ultrasound study of sinus tract formation in hidradenitis suppurativa. ermatol Online J. 2013;19:18564.
Wortsman X, Jemec GBE. Real-time compound imaging ultrasound of hidradenitis suppurativa. Dermatol Surg. 2007;33:1340-2. https://doi.org/10.1111/j.1524-4725.2007.33286.x
Jemec GBE, Gniadecka M. Ultrasound examination of hair follicles in hidradenitis. Arch Dermatol. 1997;133:967-72. https://doi.org/10.1001/archderm.1997.03890440033004
Wortsman X, Wortsman J. Ultrasound detection of retained hair tracts in hidradenitis suppurativa. Dermatol Surg. 2015;41:867-9. https://doi.org/10.1097/DSS.0000000000000388
Wortsman X, Revuz J, Jemec GBE. Lymph nodes in hidradenitis suppurativa. Dermatology. 2009;219:22-4. https://doi.org/10.1159/000213064
Martorell A, Worstman X, Alfagame F, Roustan G, Arias-Santiago S, Catalano O, et al. Ultrasound evaluation as a complementary test in hidradenitis suppurativa: Proposal of a standarize report. Dermatol Surg. 2017;43:1065-73. https://doi.org/10.1097/DSS.0000000000001147
Wortsman X, Wortsman J. Clinical usefulness of variable-frequency ultrasound in localized lesions of the skin. J Am Acad Dermatol. 2010;62:247-56. doi: 10.1016/j.jaad.2009.06.016 https://doi.org/10.1016/j.jaad.2009.06.016
Mandava A, Ravuri PR, Konathan R. High-resolution ultrasound imaging of cutaneous lesions. Indian J Radiol Imaging. 2013;23:269-77. https://doi.org/10.4103/0971-3026.120272
Beaman FD, Kransdorf MJ, Andrews TR, Murphey MD, Arcara LK, Keeling JH. Superficial soft-tissue masses: Analysis, diagnosis, and differential considerations. Radiographics. 2007;27:509-23. https://doi.org/10.1148/rg.272065082
Inampudi P, Jacobson JA, Fessell DP, Carlos RC, Patel SV, Delaney-Sathy LO, van Holsebeeck MT. Soft-tissue lipomas: Accuracy of sonography in diagnosis with pathologic correlations. Radiology. 2004;233:763-7. https://doi.org/10.1148/radiol.2333031410
Giard MC, Pineda C. Ganglion cyst versus synovial cyst? Ultrasound characteristics through a review of the literature. Rheumatol Int. 2015;35:597-605. doi: 10.1007/s00296-014-3120-1 https://doi.org/10.1007/s00296-014-3120-1
Mentes O, Oysul A, Zeybek N, Kozak O, Tufan T. Ultrasonography accurately evaluates the dimension and shape of the pylonidal sinus. Clinics (São Paulo). 2009;64:189-92. https://doi.org/10.1590/S1807-59322009000300007
Conley S. Sonographic evaluation of a pilonidal cyst: A case study. J Diagn Med Sonogr. 2016;32:279-82. https://doi.org/10.1177/8756479316662648
Tsai WC, Chiou HJ, Chou YH, Wang Hk, Chiou SY, Chang CY. Differentiation between schwannomas and neurofibromas in the extremities and superficial body: The role of high resolution and color Doppler ultrasonography. J Ultrasound Med. 2008;27:161-6. https://doi.org/10.7863/jum.2008.27.2.161
Cómo citar
Descargas
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2019 Revista de la Asociación Colombiana de Dermatología y Cirugía Dermatológica

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-CompartirIgual 4.0.
| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |







