Células de langerhans
DOI:
https://doi.org/10.29176/2590843X.1680Palabras clave:
Epidermis, Célula de Langerhans, Histiocitosis de células de Langerhans, MacrófagosResumen
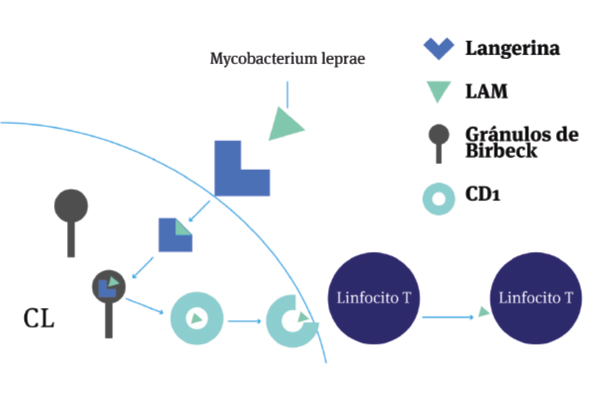
Las células de Langerhans se encuentran en las capas suprabasales de la epidermis y desempeñan un papel inmunológico importante relacionado con la vigilancia inmune, el procesamiento de antígenos y la inducción de tolerancia. Estas células poseen unas características semejantes a las células dendríticas y a los macrófagos, lo cual les aporta una gran versatilidad y les permite desarrollar funciones únicas. Por otro lado, intervienen en la patogenia de varias dermatosis desde infecciosas hasta tumorales y son un objetivo interesante para la terapia de muchas enfermedades dermatológicas
Biografía del autor/a
Leydi Yohana Gallego Vidales, Fundación Universitaria Sanitas
Residente de Dermatología, Fundación Universitaria Sanitas. Bogotá D.C, Colombia.
Martha Cecilia Valbuena Mesa, Centro Dermatológico Federico Lleras Acosta
Dermatóloga, Hospital Universitario, Centro Dermatológico Federico Lleras Acosta E.S.E. Bogotá D.C, Colombia.
Referencias bibliográficas
Langerhans P. Ueber die Nerven der menschlichen Haut. Arch Für Pathol Anat Physiol Für Klin Med.1868;44:325-37. https://doi.org/10.1007/BF01959006
Jolles S. Paul Langerhans. J Clin Pathol. 2002;55(4):243. https://doi.org/10.1136/jcp.55.4.243
Doebel T, Voisin B, Nagao K. Langerhans Cells – The Macrophage in Dendritic Cell Clothing. Trends Immunol. 2017;38(11):817-28. https://doi.org/10.1016/j.it.2017.06.008
Birbeck MS, Breathnach AS, Everall JD. An Electron Microscope Study of Basal Melanocytes and High-Level Clear Cells (Langerhans Cells) in Vitiligo*. J Invest Dermatol. 1961;37(1):51-64. https://doi.org/10.1038/jid.1961.80
Silberberg I, Baer RL, Rosenthal SA. The role of Langerhans cells in allergic contact hypersensitivity. A review of findings in man and guinea pigs. J Invest Dermatol. 1976;66(4):210-7. https://doi.org/10.1111/1523-1747.ep12482139
Steinman RM. Dendritic cells: Understanding immunogenicity. Eur J Immunol. 2007;37:S53-60. https://doi.org/10.1002/eji.200737400
Collin M, Milne P. Langerhans cell origin and regulation. Curr Opin Hematol. 2016;23(1):28-35. https://doi.org/10.1097/MOH.0000000000000202
Yan B, Liu N, Li J, Li J, Zhu W, Kuang Y, et al. The role of Langerhans cells in epidermal homeostasis and pathogenesis of psoriasis. J Cell Mol Med. 2020;24(20):11646-55. https://doi.org/10.1111/jcmm.15834
Merad M, Ginhoux F, Collin M. Origin, homeostasis and function of Langerhans cells and other langerin-expressing dendritic cells. Nat Rev Immunol. 2008;8(12):935-47. https://doi.org/10.1038/nri2455
Sparber F. Langerhans cells: an update. J Dtsch Dermatol Ges J Ger Soc Dermatol JDDG. 2014;12:1107-11. https://doi.org/10.1111/ddg.12506
Mutyambizi K, Berger CL, Edelson RL. The balance between immunity and tolerance: The role of Langerhans cells. Cell Mol Life Sci. 2009;66(5):831-40. https://doi.org/10.1007/s00018-008-8470-y
Koch S, Kohl K, Klein E, Bubnoff D von, Bieber T. Skin homing of Langerhans cell precursors: Adhesion, chemotaxis, and migration. J Allergy Clin Immunol. 2006;117(1):163-8. https://doi.org/10.1016/j.jaci.2005.10.003
Seré K, Baek J-H, Ober-Blöbaum J, Müller-Newen G, Tacke F, Yokota Y, et al. Two Distinct Types of Langerhans Cells Populate the Skin during Steady State and Inflammation. Immunity. 2012;37(5):905-16. https://doi.org/10.1016/j.immuni.2012.07.019
Clayton K, Vallejo AF, Davies J, Sirvent S, Polak ME. Langerhans Cells-Programmed by the Epidermis. Front Immunol. 2017;8:1676. https://doi.org/10.3389/fimmu.2017.01676
Ordóñez DM. Células de Langerhans en la inmunidad cutánea. Rev Asoc Col Dermatol.2007;15(4):280-5.
Mizumoto N, Takashima A. CD1a and langerin: acting as more than Langerhans cell markers. J Clin Invest. 2004;113(5):658-60. https://doi.org/10.1172/JCI21140
Kaplan DH. In vivo Function of Langerhans Cells and Dermal DC. Trends Immunol. 2010;31(12):446-51. https://doi.org/10.1016/j.it.2010.08.006
Sagi Z, Hieronymus T. The Impact of the Epithelial–Mesenchymal Transition Regulator Hepatocyte Growth Factor Receptor/Met on Skin Immunity by Modulating Langerhans Cell Migration. Front Immunol. 2018;9:517. https://doi.org/10.3389/fimmu.2018.00517
Rajesh A, Wise L, Hibma M. The role of Langerhans cells in pathologies of the skin. Immunol Cell Biol. 2019;97(8):700-13. https://doi.org/10.1111/imcb.12253
Jaitley S, Saraswathi T. Pathophysiology of Langerhans cells. J Oral Maxillofac Pathol. 2012;16(2):239-44. https://doi.org/10.4103/0973-029X.99077
Begoña Vázquez, Sureda M, Rebollo J. Células dendríticas I: aspectos básicos de su biología y funciones. Inmunología. 2012;31(1):21-30. https://doi.org/10.1016/j.inmuno.2011.10.001
Schwarz T. Inmunología. En: Callen J (editor). Dermatología. 4.a edición. España: Elsevier; 2019. p. 81-99.
Gutierrez MA. Langerhans Cells in Autoimmunity: New Perspectives in Function and Homeostasis. UCLA; 2018. Disponible en: https://t.ly/gB_iS
Kleyn CE, Schneider L, Saraceno R, Mantovani C, Richards HL, Fortune DG, et al. The Effects of Acute Social Stress on Epidermal Langerhans’ Cell Frequency and Expression of Cutaneous Neuropeptides. J Invest Dermatol. 2008;128(5):1273-9. https://doi.org/10.1038/sj.jid.5701144
Clausen BE, Romani N, Stoitzner P. Meeting Report of the 16th International Langerhans Cell Workshop: Recent Developments in Langerhans Cell and Skin Dendritic Cell Biology and their Therapeutic Application. J Invest Dermatol. 2020;140(7):1315-9. https://doi.org/10.1016/j.jid.2020.02.022
Otsuka M, Egawa G, Kabashima K. Uncovering the Mysteries of Langerhans Cells, Inflammatory Dendritic Epidermal Cells, and Monocyte-Derived Langerhans Cell-Like Cells in the Epidermis. Front Immunol. 2018;9:1768. https://doi.org/10.3389/fimmu.2018.01768
Drab M, Stopar D, Kralj-Iglič V, Iglič A. Inception Mechanisms of Tunneling Nanotubes. Cells. 2019;8(6):626. https://doi.org/10.3390/cells8060626
De La Cruz Diaz JS, Kaplan DH. Langerhans Cells Spy on Keratinocytes. J Invest Dermatol. 2019;139(11):2260-2. https://doi.org/10.1016/j.jid.2019.06.120
Abbas AK, Lichtman A, Pillai S. T Cell-Mediated Immunity: Activation of T Lymphocytes. En: Basic Immunology: Functions and Disorders of the Immune System. 6.a edición. Elsevier; 2020. pp. 96-118.
Seneschal J, Clark RA, Gehad A, Baecher-Allan CM, Kupper TS. Human epidermal Langerhans cells maintain immune homeostasis in skin by activating skin resident regulatory T cells. Immunity. 2012;36(5):873-84. https://doi.org/10.1016/j.immuni.2012.03.018
Kimber I, Cumberbatch M, Dearman RJ, Bhushan M, Griffiths CE. Cytokines and chemokines in the initiation and regulation of epidermal Langerhans cell mobilization. Br J Dermatol. 2000;142(3):401-12. https://doi.org/10.1046/j.1365-2133.2000.03349.x
Clausen BE, Kel JM. Langerhans cells: critical regulators of skin immunity? Immunol Cell Biol. 2010;88(4):351-60. https://doi.org/10.1038/icb.2010.40
Ingber A. Langerhans cell receptors. Dermatol Clin. 2007;25(4):559-62. https://doi.org/10.1016/j.det.2007.06.019
Deckers J, Hammad H, Hoste E. Langerhans Cells: Sensing the Environment in Health and Disease. Front Immunol. 2018;9:93. https://doi.org/10.3389/fimmu.2018.00093
Lemke G, Rothlin CV. Immunobiology of the TAM receptors. Nat Rev Immunol. 2008;8(5):327-36. https://doi.org/10.1038/nri2303
West HC, Bennett CL. Redefining the Role of Langerhans Cells as Immune Regulators within the Skin. Front Immunol. 2018;8:1941. https://doi.org/10.3389/fimmu.2017.01941
Su Q, Igyártó BZ. Keratinocytes Share Gene Expression Fingerprint with Epidermal Langerhans Cells via mRNA Transfer. J Invest Dermatol. 2019;139(11): 2313-23. https://doi.org/10.1016/j.jid.2019.05.006
Shklovskaya E, O’Sullivan BJ, Ng LG, Roediger B, Thomas R, Weninger W, et al. Langerhans cells are precommitted to immune tolerance induction. Proc Natl Acad Sci. 2011;108(44):18049-54. https://doi.org/10.1073/pnas.1110076108
Taguchi K, Fukunaga A, Ogura K, Nishigori C. The role of epidermal Langerhans cells in NB-UVBinduced immunosuppression. Kobe J Med Sci. 2013;59(1):E1-9.
Achachi A, Vocanson M, Bastien P, Péguet-Navarro J, Grande S, Goujon C, et al. UV Radiation Induces the Epidermal Recruitment of Dendritic Cells that Compensate for the Depletion of Langerhans Cells in Human Skin. J Invest Dermatol. 2015;135(8):2058-67. https://doi.org/10.1038/jid.2015.118
Chomiczewska-Skóra D, Adamus A, Trznadel-Grodzka E, Rotsztejn H. Effects of ultraviolet radiation on Langerhans cells. Cent Eur J Immunol. 2013;3(3):393-8. https://doi.org/10.5114/ceji.2013.37742
Schwarz A, Noordegraaf M, Maeda A, Torii K, Clausen BE, Schwarz T. Langerhans Cells Are Required for UVR-Induced Immunosuppression. J Invest Dermatol. 2010;130(5):1419-27. https://doi.org/10.1038/jid.2009.429
Kobayashi M, Tojo A. Langerhans cell histiocytosis in adults: Advances in pathophysiology and treatment. Cancer Sci. 2018;109(12):3707-13. https://doi.org/10.1111/cas.13817
Van der Vlist M, Geijtenbeek TBH. Langerin functions as an antiviral receptor on Langerhans cells. Immunol Cell Biol. 2010;88(4):410-5. https://doi.org/10.1038/icb.2010.32
Nakamine H, Yamakawa M, Yoshino T, Fukumoto T, Enomoto Y, Matsumura I. Langerhans Cell Histiocytosis and Langerhans Cell Sarcoma: Current Understanding and Differential Diagnosis. J Clin Exp Hematop. 2016;56(2):109-18. https://doi.org/10.3960/jslrt.56.109
Atmatzidis DH, Lambert WC, Lambert MW. Langerhans cell: exciting developments in health and disease. J Eur Acad Dermatol Venereol. 2017;31:1817-24. https://doi.org/10.1111/jdv.14522
Hatakeyama M, Fukunaga A, Washio K, Taguchi K, Oda Y, Ogura K, et al. Anti-Inflammatory Role of Langerhans Cells and Apoptotic Keratinocytes in Ultraviolet-B-Induced Cutaneous Inflammation. J Immunol Baltim. 2017;199(8):2937-47. https://doi.org/10.4049/jimmunol.1601681
Bulat V, Situm M, Dediol I, Ljubicić I, Bradić L. The mechanisms of action of phototherapy in the treatment of the most common dermatoses. Coll Antropol. 2011;35 Suppl 2:147-51.
Mizuno K, Okamoto H, Horio T. Ultraviolet B Radiation Suppresses Endocytosis, Subsequent Maturation, and Migration Activity of Langerhans Cell-Like Dendritic Cells. J Invest Dermatol. 2004;122(2):300-6. https://doi.org/10.1046/j.0022-202X.2004.22206.x
Fukunaga A, Khaskhely NM, Ma Y, Sreevidya CS, Taguchi K, Nishigori C, et al. Langerhans Cells Serve as Immunoregulatory Cells by Activating NKT Cells. J Immunol. 2010;185(8):4633-40. https://doi.org/10.4049/jimmunol.1000246
Sarmiento L, Peña S. La célula de Langerhans. Biomédica. 2002;22(4):462-5. https://doi.org/10.7705/biomedica.v22i4.1172
Cómo citar
Descargas
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2023 Revista de la Asociación Colombiana de Dermatología y Cirugía Dermatológica

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-CompartirIgual 4.0.

| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |






