Plaque psoriasis secondary to the use of tyrosine kinase inhibitors, a case report and narrative review of the literature
DOI:
https://doi.org/10.29176/2590843X.1727Keywords:
Chronic myeloid leukemia, Dasatinib, Imatinib, Nilotinib, PsoriasisAbstract
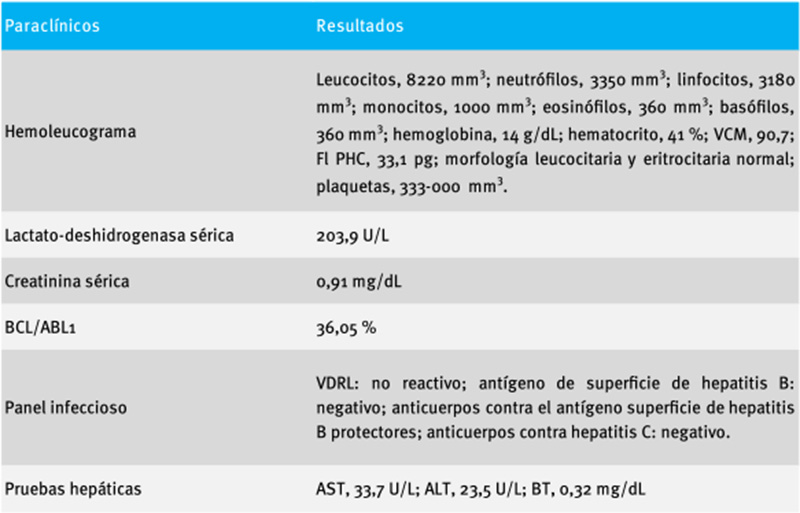
Tyrosine kinase inhibitors, used as the first line for treating chronic myeloid leukemia (CML)-Philadelphia chromosome positive, have been associated with the development of cutaneous adverse effects, where lesions compatible with psoriasis have been described. We present the case of a 55-year-old man with a history of CML-Philadelphia chromosome positive, with no personal or family history of psoriasis. However, he developed plaque psoriasis 2 years after starting treatment with this group of medications (imatinib and dasatinib). A narrative review of the literature on psoriasis triggered by tyrosine kinase inhibitors was conducted, and other cutaneous adverse effects probably caused by these drugs are described.
References
Vargas GA, Ramírez C, Gómez F, Peña MN, Vasco C, Medina LJ, et al. Características clínicas y respuesta a la fototerapia de los pacientes con psoriasis. 2018;26(2):106-15. https://doi.org/10.29176/2590843X.46
Daudén E, Pujol RM, Sánchez-carazo JL, Toribio J, Vanaclocha F, Puig L, et al. Demographic characteristics and health-related quality of life of patients with moderate-to-severe psoriasis: The VACAP study. Actas Dermosifiliogr. 2013;104(9):807-14. https://doi.org/10.1016/j.ad.2013.03.005
Rachakonda TD, Schupp CW, Armstrong AW. Psoriasis prevalence among adults in the United States. J Am Acad Dermatol. 2014;70(3):512-6. https://doi.org/10.1016/j.jaad.2013.11.013
González C, Castro LA, Cruz GD, Arenas CM, Beltrán A, Santos AM. Caracterización epidemiológica de la psoriasis en el Hospital Militar Central. Rev Asoc Colomb Dermatol Cir Dermatol. 2009;17(1):11-7.
Sanclemente G, Mahecha M, Guzmán C. Enfermedades de la piel más frecuentes dermatológicas del Hospital Universitario San Vicente de Paúl y del Hospital Infantil, Medellín, Colombia 1999. Acta Med Colomb. 2001;26(5):240-5.
Nestle FO, Kaplan DH, Barker J. Psoriasis. N Engl J Med. 2009;361(5):496-509. https://doi.org/10.1056/NEJMra0804595. PMID: 19641206
Carella AM, Saglio G, Mahon XF, Mauro MJ. Present results and future perspectives in optimizing chronic myeloid leukemia therapy. Haematologica. 2018;103(6):928-30. https://doi.org/10.3324/haematol.2017.182022
Wei X, He L, Wang X, Lin M, Dai J. Effects of dasatinib on CD8+ T, Th1, and Treg cells in patients with chronic myeloid leukemia. J Int Med Res. 2020;48(2):30006051987732. https://doi.org/10.1177/0300060519877321
Brown G, Wang E, Leon A, Huynh M, Wehner M, Matro R, et al. Tumor necrosis factor-α inhibitor-induced psoriasis: Systematic review of clinical features, histopathological findings, and management experience. J Am Acad Dermatol. 2017;76(2):334-41. http://doi.org/10.1016/j.jaad.2016.08.012
Balak D, Hajdarbegovic E. Drug-induced psoriasis: clinical perspectives. Psoriasis (Auckl). 2017;7:87-94. http://doi.org/10.2147/PTT.S126727
Armstrong AW. Psoriasis provoked or exacerbated by medications: Identifying culprit drugs. JAMA Dermatol. 2014;150(9):963. http://doi.org/10.1001/jamadermatol.2014.1019
Woo SM, Huh CH, Park KC, Youn SW. Exacerbation of psoriasis in a chronic myelogenous leukemia patient treated with imatinib. J Dermatol. 2007;34(10):724-6. https://doi.org/10.1111/j.1346-8138.2007.00369.x
Figueiredo Brandao BJ, Arjona Aguilera C, Jiménez Gallo D, Linares Barrios M. Psoriasis inducida por imatinib. Piel. 2017;32(3):136-8. https://doi.org/10.1016/j.piel.2016.06.010
Jain A. Imatinib Induced Complete Remission of Psoriasis in a Patient with Chronic Myeloid Leukemia. Indian J Hematol Blood Transfus. 2020;36(1):198-9. https://doi.org/10.1007/s12288-019-01162-1
Miyagawa S, Fujimoto H, Ko S, Hirota S, Kitamura Y. Improvement of psoriasis during imatinib therapy in a patient with a metastatic gastrointestinal stromal tumour. Br J Dermatol. 2002;147(2):406-7. https://doi.org/10.1046/j.1365-2133.2002.497217.x
Navarro R, Daudén E. Reacciones psoriasiformes paradójicas durante el tratamiento con terapia anti-factor de necrosis tumoral. Manejo clínico. Actas Dermosifiliogr. 2014;105(8):752-61. https://doi.org/10.1016/j.ad.2013.05.007
De Gannes GC, Ghoreishi M, Pope J, Russell A, Bell D, Adams S, et al. Psoriasis and pustular dermatitis triggered by TNF-α inhibitors in patients with rheumatologic conditions. Arch Dermatol. 2007;143(2):223-31. https://doi.org/10.1001/archderm.143.2.223
Montolio Chiva L, Martínez Ferrer À, Mateu Puchades A, Campos Fernández C, Narváez Garcia J, Alegre Sancho JJ. Psoriasis inducida por terapia biológica. Reumatol Clin. 2021;17(8):437-9. https://doi.org/10.1016/j.reuma.2019.12.005
Ramírez LC, Velásquez MM. Aspectos de la IL-17 en la inmunopatogénesis de la psoriasis: un nuevo blanco terapéutico. Rev Asoc Colomb Dermatol. 2015;23(1):61-8.
Armstrong AW, Read C. Pathophysiology, Clinical Presentation, and Treatment of Psoriasis: A Review. JAMA. 2020;323(19):1945-60. https://doi.org/10.1001/jama.2020.4006
Seggewiss R, Loré K, Greiner E, Magnusson MK, Price DA, Douek DC, et al. Imatinib inhibits Tcell receptor-mediated T-cell proliferation and activation in a dose-dependent manner. Blood. 2005;105(6):2473-9. https://doi.org/10.1182/blood-2004-07-2527
Thachil J. T-regulatory cell response in psoriasis and changes with imatinib therapy. Clin Exp Dermatol. 2009;34(8):e1022. https://doi.org/10.1111/j.1365-2230.2009.03696.x
Nagai T, Karakawa M, Komine M, Muroi K, Ohtsuki M, Ozawa K. Development of psoriasis in a patient with chronic myelogenous leukaemia during nilotinib treatment. Eur J Haematol. 2013;91(3):270-2. https://doi.org/10.1111/ejh.12153
Musolino C, Allegra A, Mannucci C, Russo S, Alonci A, Maisano V, et al. matinib Mesilat ile li kili Deri Toksisitesinde nterlökin-31/33 Aksının Olası Rolü. Turkish J Hematol. 2015;32(2):168-71. https://doi.org/10.4274/Tjh.2014.0021
Mühl S, Ehrchen J, Metze D. Blistering and Skin Fragility Due to Imatinib Therapy: Loss of Laminin and Collagen IV as a Possible Cause of Cutaneous Basement Membrane Instability. Am J Dermatopathol. 2018;40(5):371-4. https://doi.org/10.1097/DAD.0000000000001063
Lee WJ, Lee JH, Won CH, Chang SE, Choi JH, Moon KC, et al. Clinical and histopathologic analysis of 46 cases of cutaneous adverse reactions to imatinib. Int J Dermatol. 2016;55(5):e268-74. https://doi.org/10.1111/ijd.13111
Ugurel S, Hildenbrand R, Dippel E, Hochhaus A, Schadendorf D. Dose-dependent severe cutaneous reactions to imatinib. Br J Cancer. 2003;88(8):1157-9. https://doi.org/10.1038/sj.bjc.6600893
Finlay AY. Current severe psoriasis and the rule of tens. Br J Dermatol. 2005;152(5):861-7. https://doi.org/10.1111/j.1365-2133.2005.06502.x
Castro Ayarza JR, Franco MD, González CF, Londoño MA. Guía de práctica clínica para el tratamiento de la psoriasis en Colombia. Actualización 2022. Asociación Colombiana de Dermatología y Cirugía Dermatológica; 2022. En publicación.
Florek AG, Wang CJ, Armstrong AW. Treatment preferences and treatment satisfaction among psoriasis patients: a systematic review. Arch Dermatol Res. 2018;310:271-319. http://dx.doi.org/10.1007/s00403-018-1808-x
Thekkudan SF, Nityanand S. Development of Psoriasis Vulgaris in a Chronic Myeloid Leukemia Patient on Second-Generation Tyrosine Kinase Inhibitor Therapy. J L
Atalay F, Kilkiliç E, Ada S. Imatinib-induced psoriasis. Turkish J Hematol. 2013;30(2):216-8. https://doi.org/10.4274/Tjh.2012.0147
Shim JH, Oh SH, Jun JY, Kim JH, Park HY, Park JH, et al. Exacerbation of psoriasis after imatinib mesylate treatment. Ann Dermatol. 2016;28(3):409-11. https://doi.org/10.5021/ad.2016.28.3.409
Kaur S, Kaur Arora A, Sekhon J, Sood N. Nilotinibinduced psoriasis in a patient of chronic myeloid leukemia responding to methotrexate. Indian J Dermatol Venereol Leprol. 2015;81(2):214-6. https://doi.org/10.4103/0378-6323.152311
Cheng H, Geist DE, Piperdi M, Virk R, Piperdi B. Management of imatinib-related exacerbation of psoriasis in a patient with a gastrointestinal stromal tumour. Australas J Dermatol. 2009;50(1):41-3. https://doi.org/10.1111/j.1440-0960.2008.00495.x
Dickens E, Lewis F, Bienz N. Imatinib: A designer drug, another cutaneous complication. Clin Exp Dermatol. 2009;34(5):603-4. https://doi.org/10.1111/j.1365-2230.2009.03250.x
Shi CR, Nambudiri VE. Imatinib-induced psoriasiform eruption in a patient with chronic myeloid leukemia. Am J Hematol. 2018;93(3):467-8. https://doi.org/10.1002/ajh.24894
Brazzelli V, Grasso V, Borroni G. Imatinib, dasatinib and nilotinib: A review of adverse cutaneous reactions with emphasis on our clinical experience. J Eur Acad Dermatol Venereol. 2013;27(12):1471-80. https://doi.org/10.1111/jdv.12172
Pretel-Irazabal M, Tuneu-Valls A, OrmaecheaPérez N. Adverse skin effects of imatinib, a tyrosine kinase inhibitor. Actas Dermosifiliogr. 2014;105(7):655-62. http://doi.org/10.1016/j.ad.2013.01.009
Dervis E, Ayer M, Belli AA, Barut SG. Cutaneous adverse reactions of imatinib therapy in patients with chronic myeloid leukemia: A six-year follow up. Eur J Dermatol. 2016;26(2):133-7. http://doi.org/10.1684/ejd.2015.2684
Drucker AM, Wu S, Busam KJ, Berman E, AmitayLaish I, Lacouture ME. Rash with the multitargeted kinase inhibitors nilotinib and dasatinib: Metaanalysis and clinical characterization. Eur J Haematol. 2013;90(2):142-50. http://doi.org/10.1111/ejh.12052
Valeyrie L, Bastuji-Garin S, Revuz J, Bachot N, Wechsler J, Berthaud P, et al. Adverse cutaneous reactions to imatinib (STI571) in Philadelphia chromosome-positive leukemias: A prospective study of 54 patients. J Am Acad Dermatol. 2003;48(2):201-6. http://doi.org/10.1067/mjd.2003.44
Vinay K, Yanamandra U, Dogra S, Handa S, Suri V, Kumari S, et al. Long-term mucocutaneous adverse effects of imatinib in Indian chronic myeloid leukemia patients. Int J Dermatol. 2018;57(3):332-8. http://doi.org/10.1111/ijd.13852
Khokar A, Malik U, Butt G, Naumeri F. Cutaneous manifestations in chronic myeloid leukemia in chronic phase treated with imatinib. Int J Dermatol. 2019;58(9):1098-101. http://doi.org/10.1111/ijd.14562
Llamas-Velasco M, Fraga J, Kutzner H, Steegmann JL, García-Diez A, Requena L. Hypopigmented macules secondary to imatinib for the treatment of chronic myeloid leukemia: A histopathologic and immunohistochemical study. J Cutan Pathol. 2014;41(5):417-26. http://doi.org/10.1111/cup.12298
Delgado L, Giraudier S, Ortonne N, Zehou O, Cordonnier C, Hulin A, et al. Adverse cutaneous eactions to the new second-generation tyrosine kinase inhibitors (dasatinib, nilotinib) in chronic myeloid leukemia. J Am Acad Dermatol. 2013;69(5):839-40. https://doi.org/10.1016/j.jaad.2013.07.025
Gonçalves Basso F, Cominato Boer C, Pizzigatti Corrêa ME, Torrezan M, Cintra ML, De Magalhães MHCG, et al. Skin and oral lesions associated to imatinib mesylate therapy. Support Care Cancer. 2009;17(4):465-8. http://doi.org/10.1007/s00520-008-0536-8
Tarantini F, Anelli L, Ingravallo G, Attolico I, Zagaria A, Rossi AR, et al. Skin lesions in chronic myeloid leukemia patients during dasatinib treatment. Cancer Manag Res. 2019;11:7991-6. http://doi.org/10.2147/CMAR.S217872
Kuraishi N, Nagai Y, Hasegawa M, Ishikawa O. Lichenoid drug eruption with palmoplantar yperkeratosis due to imatinib mesylate: A case report and a review of the literature. Acta Derm Venereol. 2010;90(1):73-6. http://doi.org/10.2340/00015555-0758
Llamas-Velasco M, Ovejero-Merino E, García-Diez A, Requena L, Daudén E, Steegmann JL. Cutaneous side effects in a cohort of patients with chronic myeloid leukemia treated with tyrosine kinase inhibitors: General description and further characterization, correlation with photoexposition and study of hypopigmentation as treatment’s prognostic factor. Dermatol Ther. 2020;33(6):e14428. http://doi.org/10.1111/dth.14428
Breccia M, Carmosino I, Russo E, Morano SG, Latagliata R, Alimena G. Early and tardive skin adverse events in chronic myeloid leukaemia patients treated with imatinib. Eur J Haematol. 2005;74(2):121-3. http://doi.org/10.1111/j.1600-0609.2004.00351.x
How to Cite
Downloads
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Revista de la Asociación Colombiana de Dermatología y Cirugía Dermatológica

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |






