Lupus panniculitis
DOI:
https://doi.org/10.29176/2590843X.318Keywords:
Panniculitis, lupus erythematosus, lupus erythematosuscutaneous, lymphoma, T-cellAbstract
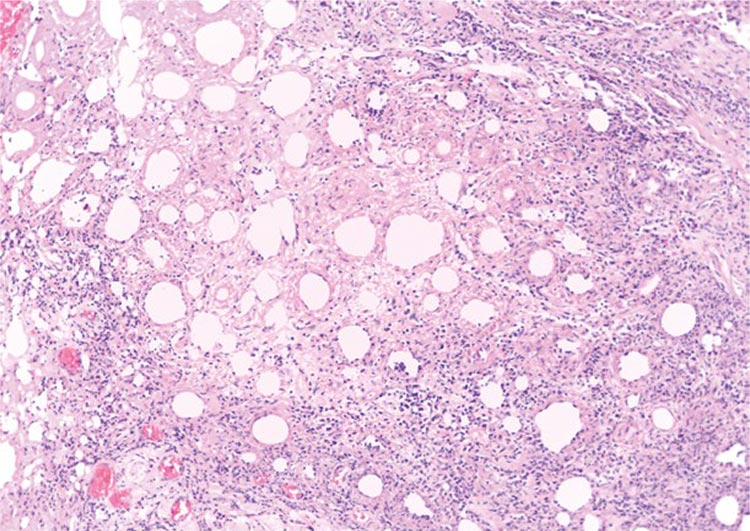
Lupus panniculitis is a subtype of cutaneous lupus with an autoimmune etiology that may be related to other forms of cutaneous lupus, SLE and other autoimmune diseases. Clinically and histologically it may be diagnosed as subcutaneous panniculitis-like T-cell lymphoma. Treatment of this type of panniculitis has not been standardized given the low prevalence of the disease. We review the epidemiological, histopathological, clinical, and therapeutic aspects of lupus panniculitis.
Author Biographies
Luis Fernando González
Médico dermatólogo, programa de Dermatologia, Universidad El Bosque, Bogotá, D.C., Colombia
Yenny Estupiñán Salazar
Médico, residente de Dermatología de segundo año, Servicio de Dermatología, Hospital Simón Bolívar, Universidad El Bosque,
Bogotá, D.C., Colombia
Fernando Vela
Médico internista, especialista en Reumatología, Universidad Nacional de Colombia, Bogotá, D.C., Colombia
Adriana Motta
Médica dermatóloga, especialista en Epidemiología; jefe, Servicio de Dermatología, Hospital Simón Bolívar, Universidad El Bosque, Bogotá, D.C., Colombia
Mariam Rolón
Médica dermatóloga, especialista en Dermatopatología, Servicio de Patología, Hospital Simón Bolívar, Bogotá, D.C., Colombia
References
Arnold HL.Lupus erythematosus profundus (Kaposi-Irgang) historical review and report of a case. Arch Derm Syphilol. 1948;57:196-203.
https://doi.org/10.1001/archderm.1948.01520140058007
Irgang S. Lupus erythematosus profundus: Report of an example with clinical resemblance to Darier-Roussy sarcoid. Arch Dermat Syph. 1940;42:97-108.
https://doi.org/10.1001/archderm.1940.01490130101012
Arnold HL. Lupus erythematosus profundus; commentary and report of four more cases. AMA Arch Derm. 1956;73:15-33.
https://doi.org/10.1001/archderm.1956.01550010017002
Fountain RB. Lupus erythematosus profundus. Br J Dermatol. 1968;80:571-9.
https://doi.org/10.1111/j.1365-2133.1968.tb12355.x
Winkelmann RK. Panniculitis and systemic lupus erythematosus. JAMA. 1970;211:472-5.
https://doi.org/10.1001/jama.1970.03170030064009
Tuffanelli DL. Lupus erythematosus panniculitis (profundus): Clinical and immunologic studies. Arch Dermatol. 1971;103:231-42.
https://doi.org/10.1001/archderm.1971.04000150001001
Fraga J, García-Díez A. Lupus erythematosus panniculitis. Dermatol Clin. 2008;26:453-63.
https://doi.org/10.1016/j.det.2008.06.002
Massone C, Kodama K, Salmhofer W, Abe R, Shimizu H, Parodi A, et al. Lupus erythematosus panniculitis (lupus profundus): Clinical, histopathological, and molecular analysis of nine cases. J Cutan Pathol. 2005;32:396-404.
https://doi.org/10.1111/j.0303-6987.2005.00351.x
Martens PB, Moder KG, Ahmed I. Lupus panniculitis: Clinical perspectives from a case series. J Rheumatol. 1999;26:68-72.
De la Moneda Herrerin C, Conde Zurita JM, Guerra Tapia A. El lupus paniculitis: una paniculitis mixta. Actas Dermosifiliogr. 1987;78:229-38.
Peters MS, Su WP. Lupus erythematosus panniculitis. Med Clin North Am. 1989;73:1113-25.
https://doi.org/10.1016/S0025-7125(16)30622-8
Tuffanelli DL. Lupus erythematosus (panniculitis) profundus: A classic revisited commentary and report of 22 cases. Hawaii Med J. 1992;41:394-7.
Magro CM, Crowson AN, Kovatich AJ, Burns F. Lupus profundus, indeterminate lymphocytic lobular panniculitis and subcutaneous T-cell lymphoma: A spectrum of subcuticular T-cell lymphoid dyscrasia. J Cutan Pathol. 2001;28:235-47.
https://doi.org/10.1034/j.1600-0560.2001.028005235.x
Nousari HC, Kimyai-Asadi A, Provost TT. Generalized lupus erythematosus profundus in a patient with genetic partial deficiency of C4. J Am Acad Dermatol. 1999;41:362-4.
https://doi.org/10.1016/S0190-9622(99)70389-0
Wenzel J, Tüting T. Identification of type I interferon-associated inflammation in the pathogenesis of cutaneous lupus erythematosus opens up options for novel therapeutic approaches. Exp Dermatol. 2007;16:454-63.
https://doi.org/10.1111/j.1600-0625.2007.00556.x
Wenzel J, Proelss J, Wiechert A, Zahn S, Bieber T, Tüting T. CXCR3-mediated recruitment of cytotoxic lymphocytes in lupus erythematosus profundus. J Am Acad Dermatol. 2007;56:648-50.
https://doi.org/10.1016/j.jaad.2006.08.014
Abreu-Velez AM, Loebl AM, Howard MS. Autoreactivity to sweat and sebaceous glands and skin homing T cells in lupus profundus. Clin Immunol. 2009;132:420-4.
https://doi.org/10.1016/j.clim.2009.05.009
Tuffanelli DL. Lupus panniculitis. Semin Dermatol. 1985;4:79-81.
Patterson JW. Panniculitis. En: Bologna JL, Jorizzo JL, Rapini RP, editores. Dermatology. Londres: Mosby; 2010. p. 1653-4.
Klein SA, Tomaro AJ. Lupus erythematosus profundus: Review of the literature and report of case. J Oral Surg. 1975;33:454-7.
Carducci M, Mussi A, Lisi S, Muscardin L, Solivetti FM. Lupus mastitis: A 2-year history of a single localization of lupus erythematosus mimicking breast carcinoma. J Eur Acad Dermatol Venerol. 2005;19:260-2.
https://doi.org/10.1111/j.1468-3083.2005.01030.x
Sabaté JM, Gómez A, Torrubia S, Salinas T, Clotet M, Lerma E. Lupus paniculitis involving the breast. Eur Radiol. 2006;16:53-6.
https://doi.org/10.1007/s00330-005-2810-1
White WL, Sherertz EF, Berg D, Clark RE. Periparotid lupus erythematosus panniculitis: Clinic pathologic correlation of two cases presenting as primary parotid disease. Arch Pathol Lab Med. 1993;117:535-9.
Ogura N, Fujisaku A, Jodo S, Ichikawa K, Tsutsumi A, Mukai M, et al. Lupus erythematosus profundus around the salivary glands: A case resembling submandibular gland disease. Lupus. 1997;6:477-9.
https://doi.org/10.1177/096120339700600512
Sardana K, Mendiratta V, Koranne RV, Verma R, Vig R. Lupus erythematosus profundus involving the ear lobe. J Eur Acad Dermatol Venerol. 2003;17:727-9.
https://doi.org/10.1046/j.1468-3083.2003.00824.x
Tamada Y, Arisawa S, Ikeya T, Yokoi T, Hara K, Matsumoto Y. Linear lupus erythematosus profundus in a young man. Br J Dermatol. 1999;140:177-8.
https://doi.org/10.1046/j.1365-2133.1999.02636.x
Nagai Y, Ishikawa O, Hattori T, Ogawa T. Linear lupus erythematosus profundus on the scalp following the lines of Blaschko. Eur J Dermatol. 2003;13:294-6.
Chan I, Robson A, Mellerio JE. Multiple dermatofibromas associated with lupus profundus. Clin Exp Dermatol. 2005;30:128-30.
https://doi.org/10.1111/j.1365-2230.2004.01663.x
García-Doval I, Roson E, Abalde M, Feal C, Cruces MJ. Coexistence of acquired localized hypertrichosis and lipoatrophy after lupus panniculitis. J Am Acad Dermatol. 2004;50:799-800.
https://doi.org/10.1016/j.jaad.2003.08.020
Nousari HC, Kimyai-Asadi A, Provost TT.Generalized lupus erythematosus profundus in a patient with genetic partial deficiency of C4. J Am Acad Dermatol. 1999;41:362-4.
https://doi.org/10.1016/S0190-9622(99)70389-0
Cribier B. Panniculite lupique. Presse Med. 2005;34:243-8.
https://doi.org/10.1016/S0755-4982(05)88257-0
Patterson JW. Panniculitis. En: Weedon D, Geoffrey S, Adam IR, editors. Weedon's Skin Pathology. Edinburgh: Churchill Livingstone/Elsevier, 2010. p. 542-3.
Patterson JW. Differential diagnosis of panniculitis. Adv Dermatol. 1991;6:309-29.
Barnhill RL, Crowson AN. Panniculitis. Textbook of Dermatopathology. 2nd edition. New York: McGraw-Hill; 2004. p. 267-98.
Arai S, Katsuoka K. Clinical entity of lupus erythematosus panniculitis/lupus erythematosus profundus. Autoimmunity Reviews. 2009;8:449-52.
https://doi.org/10.1016/j.autrev.2008.12.011
Luzar C. Inflammatory diseases of cutaneous fat: Lupus erythematosus profundus. En: Calonje E, Brenn T, Lazar A, McKee PH, editors. McKee's pathology of the skin: with clinical correlations. 4th ed. Edinburgh: Elsevier/Saunders; 2012. p. 358-360.
Hansen CB, Callen JP. Connective tissue panniculitis: Lupus panniculitis, dermatomyositis, morphea/scleroderma. Dermatol Ther. 2010;23: 341-9.
https://doi.org/10.1111/j.1529-8019.2010.01334.x
Cusack CA, Fanelli M. Panniculitis. En: Lebwohl MG, Heymann WR, Berth-Jones J, eitors. Treatment of Skin Diseases: Comprehensive Therapeutic Strategies. Fourt edition. Philaderphia: Saunders; 2013. p. 528-9.
Braunstein I, Werth VP. Update on management of connective tissue panniculitides. Dermatol Ther. 2012;25:173-82.
https://doi.org/10.1111/j.1529-8019.2012.01489.x
Kuhn A, Landmann A. The classification and diagnosis of cutaneous lupus erythematosus. J Autoimmun. 2014;48-49:14-9.
https://doi.org/10.1016/j.jaut.2014.01.021
Ziemer M, Milkova L, Kunz M. Lupus erythematosus. Part II: Clinical picture, diagnosis and treatment. J Dtsch Dermatol Ges. 2014;12:285-301.
https://doi.org/10.1111/ddg.12254
Morgan KW, Callen JP. Calcifying lupus panniculitis in a patient with subacute cutaneous lupus erythematosus: Response to diltiazem and chloroquine. J Rheumatol. 2001;28:2129-32.
Chatham WW, Kimberly RP. Treatment of lupus with corticosteroids. Lupus. 2001;10:140-7.
https://doi.org/10.1191/096120301675075008
Yell JA, Burge SM. Lupus erythematosus profundus treated with clobetasol propionate under a hydrocolloid dressing. Br J Dermatol. 1993;128:103.
https://doi.org/10.1111/j.1365-2133.1993.tb00158.x
González-Sixto B, García-Doval I, Oliveira R, Posada C, García-Cruz MA, Cruces M. Quinacrine in the treatment of cutaneous lupus erythematosus: Practical aspects and a case series. Actas Dermosifiliogr. 2010;101:54-8.
https://doi.org/10.1016/j.ad.2009.07.002
Page F. Treatment of lupus erythematosus with mepacrine. Lancet. 1951;2:755-8.
https://doi.org/10.1016/S0140-6736(51)91643-1
Chung HS, Hann SK. Lupus panniculitis treated by a combination therapy of hydroxychloroquine and quinacrine. J Dermatol. 1997;24:569-72.
https://doi.org/10.1111/j.1346-8138.1997.tb02294.x
Yang CS, Kim C, Antaya R. Review of thalidomide use in the pediatric population. J Am Acad Dermatol. 2015;72:703-11.
https://doi.org/10.1016/j.jaad.2015.01.002
Wienart S, Gadola S, Hunziker T. Facets of lupus erythematosus: Panniculitis responding to thalidomide. J Dtsch Dermatol Ges. 2008;6:214-6.
https://doi.org/10.1111/j.1610-0387.2007.06525.x
Burrows NP, Walport MJ, Hammond AH, Davey N, Jones RR. Lupus erythematosus profundus with partial C4 deficiency responding to thalidomide. Br J Dermatol. 1991;125:62-7.
https://doi.org/10.1111/j.1365-2133.1991.tb06042.x
Hansen CB, Dahle KW. Cutaneous lupus erythematosus. Dermatol Ther. 2012;25:99-111.
https://doi.org/10.1111/j.1529-8019.2012.01508.x
Cortés-Hernández J, Torres-Salido M, Castro-Marrero J, Vilardell-Tarres M, Ordi-Ros J. Thalidomide in the treatment of refractory cutaneous lupus erythematosus: Prognostic factors of clinical outcome. Br J Dermatol. 2012;166:616-23.
https://doi.org/10.1111/j.1365-2133.2011.10693.x
Ujiie H, Shimizu T, Ito M, Arita K, Shimizu H. Lupus erythematosus profundus successfully treated with dapsone: Review of the literature. Arch Dermatol. 2006:142:399-401.
https://doi.org/10.1001/archderm.142.3.399
Samuelsson A, Towers TL, Ravetch JV. Anti-inflammatory activity of IVIG mediated through the inhibitory Fc receptor. Science. 2001;291:484
https://doi.org/10.1126/science.291.5503.484
Fehr J, Hoffman V, Kappeler U. Transient reversal of thrombocytopenia in idiopathic thrombocytopenic purpura by high-dose intravenous gamma globulin. N Engl J Med. 1982;306:1254.
https://doi.org/10.1056/NEJM198205273062102
Santo JE, Gomes MF, Gomes MJ, Peixoto LC, Pereira S, Acabado A, et al. Intravenous immunoglobulin in lupus panniculitis. Clin Rev Allergy Immunol. 2010;38:307-18.
https://doi.org/10.1007/s12016-009-8162-x
Moreno-Suárez F, Pulpillo-Ruiz A. Rituximab for the treatment of lupus erythematosus panniculitis. Dermatol Ther. 2013;26:415-8.
https://doi.org/10.1111/dth.12014
McArdle A, Baker JF. A case of "refractory" lupus erythematosus profundus responsive to rituximab. ClinRheumatol. 2009;28:745-6.
https://doi.org/10.1007/s10067-009-1158-3
Wozniacka A, Salamon M, Lesiak A, McCauliffe DP, Sysa-Jedrzejowska A. The dynamism of cutaneous lupus erythematosus: Mild discoid lupus erythematosus evolving into SLE with SCLE and treatment resistant lupus panniculitis. Clin Rheumatol. 2007;26:1176-9.
https://doi.org/10.1007/s10067-006-0310-6
Kuhn A, Ruland V, Bonsmann G. Cutaneous lupus erythematosus: Update of therapeutic options. Part II. J Am Acad Dermatol. 2011;65:195-213.
https://doi.org/10.1016/j.jaad.2010.06.017
Saeki Y, Ohshima S, Kurimoto I, Miura H, Suemura M. Maintaining remission of lupus erythematosus profundus (LEP) with cyclosporin A. Lupus. 2000;9:390-2.
https://doi.org/10.1191/096120300678828406
Ishiguro N, Iwasaki T, Kawashima M, Kawakami M. Intractable ulceration in a patient with lupus erythematosus profundus successfully treated with cyclosporine. Int J Dermatol. 2012; 51:1131-3.
https://doi.org/10.1111/j.1365-4632.2010.04746.x
Günther C, Aringer M, Lochno M, Kämmerer E, Bauer A, Wozel G, et al. TNF-alpha blockade with infliximab in a patient with lupus erythematosus profundus. Acta Derm Venereol. 2012;92:401-3.
https://doi.org/10.2340/00015555-1262
Lee H, Kim DS, Chung KY. Adalimumab-induced lupus panniculitis. Lupus. 2014;23:1443-4.
https://doi.org/10.1177/0961203314545411
Winkelmann RR, Kim GK, Del Rosso JQ. Treatment of cutaneous lupus erythematosus: Review and assessment of treatment benefits based on Oxford Centre for evidence-based medicine. J Clin Aesthet Dermatol. 2013;6:27-38.
Boehm IB, Boehm GA, Bauer R. Management of cutaneous lupus erythematosus with low-dose methotrexate: Indication for modulation of inflammatory mechanisms. Rheumatol Int. 1998;18:59-62.
https://doi.org/10.1007/s002960050058
Eastham AB, Liang CA, Femia AN, Lee TC, Vleugels RA, Merola JF. Lupus erythematosus panniculitis-induced facial atrophy: effective treatment with poly-L-lactic acid and hyaluronic acid dermal fillers. J Am Acad Dermatol. 2013;69:260-2.
How to Cite
Downloads
Downloads
Published
How to Cite
Issue
Section

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |






