Diagnostic and treatment management of patients with pemphigus vulgaris and foliaceus
DOI:
https://doi.org/10.29176/2590843X.1884Keywords:
Blister, Fluorescent antibody technique, direct, Pemphigus, Rituximab, Skin diseases, VesiculobullousAbstract
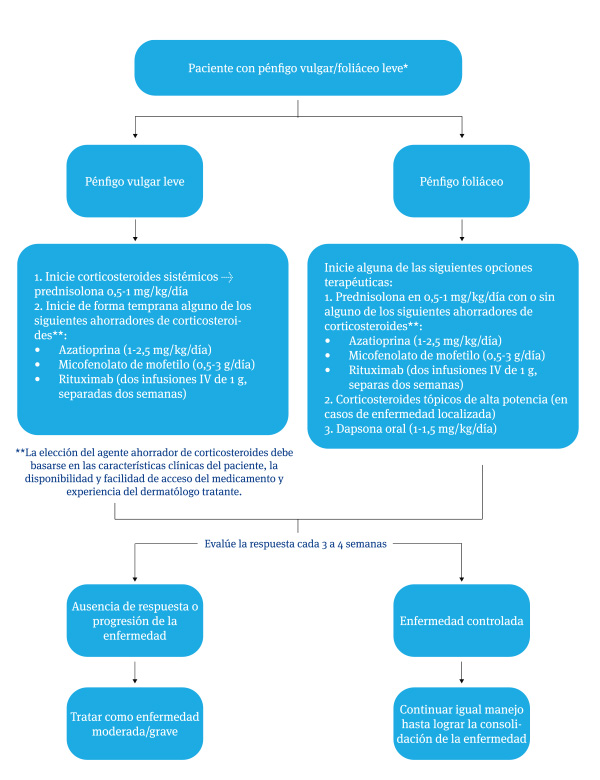
Introduction: Pemphigus are rare, but potentially serious, autoimmune blistering diseases that can be associated with catastrophic consequences if an appropriate diagnostic and therapeutic approach is not performed. The Dermatology service of the University of Antioquia at its main headquarters, Hospital Alma Mater de Antioquia and Hospital Universitario San Vicente Fundación, is a reference center for the study and management of these diseases. Methodology: review of the literature and socialization in the group of teachers and residents of the University of Antioquia to develop management guidelines. Results: Guidelines are described in the diagnosis and treatment of patients with pemphigus vulgaris and pemphigus foliaceus. Likewise, a narrative review of the scientific evidence that supports what is recommended in this article is carried out.
Author Biographies
Camilo Ruiz, Universidad de Antioquia, Medellín, Colombia.
Residente dermatología Universidad de Antioquia
Jennifer Arenas Sepúlveda, Universidad de Antioquia, Medellín, Colombia.
Residente dermatología Universidad de Antioquia
Erika Patricia Muñoz Herrera, Universidad de Antioquia, Medellín, Colombia.
Residente dermatología Universidad de Antioquia
H, Universidad de Antioquia
Residente dermatología Universidad de Antioquia
Daniela Astarot Uribe Salazar, Universidad de Antioquia, Medellín, Colombia.
Residente dermatología Universidad de Antioquia
José Tomás Peralta Fuentes, Universidad de Antioquia, Medellín, Colombia.
Residente dermatología Universidad de Antioquia
Marcos Stivel Munera Patiño, Universidad de Antioquia, Medellín, Colombia.
Residente dermatología Universidad de Antioquia
Paula Andrea Aristizabal Diaz, Universidad de Antioquia, Medellín, Colombia.
Residente dermatología Universidad de Antioquia
Santiago Beuth Ruiz, Universidad de Antioquia, Medellín, Colombia.
Residente dermatología Universidad de Antioquia
Margarita María Velásquez Lopera, Universidad de Antioquia, Medellín, Colombia.
Servicio de Dermatología, Facultad de Medicina, Universidad de Antioquia.
Gloria Andrea Vargas Suaza, Universidad de Antioquia, Medellín, Colombia.
Servicio de Dermatología, Facultad de Medicina, Universidad de Antioquia.
Claudia Patricia Palacios Isaza, Universidad de Antioquia, Medellín, Colombia.
Servicio de Dermatología, Facultad de Medicina, Universidad de Antioquia.
Carlos Eduardo Montealegre Gómez, Universidad de Antioquia, Medellín, Colombia.
Servicio de Dermatología, Facultad de Medicina, Universidad de Antioquia.
Oscar Jairo Valencia Ocampo, Universidad de Antioquia, Medellín, Colombia.
Servicio de Dermatología, Facultad de Medicina, Universidad de Antioquia.
Manuel Antonio Martínez Gómez, Universidad de Antioquia, Medellín, Colombia.
Servicio de Dermatología, Facultad de Medicina, Universidad de Antioquia.
Miguel Mateo Cuervo López, Universidad de Antioquia, Medellín, Colombia.
Servicio de Dermatología, Facultad de Medicina, Universidad de Antioquia.
Alberto de Jesús Uribe Correa, Universidad de Antioquia, Medellín, Colombia.
Servicio de Dermatología, Facultad de Medicina, Universidad de Antioquia.
Juan David Ruiz Restrepo, Universidad de Antioquia, Medellín, Colombia.
Servicio de Dermatología, Facultad de Medicina, Universidad de Antioquia.
Juan Pablo Ospina Gómez, Universidad de Antioquia, Medellín, Colombia.
Servicio de Dermatología, Facultad de Medicina, Universidad de Antioquia.
Luis Alfonso Correa Londoño, Universidad de Antioquia, Medellín, Colombia.
Servicio de Dermatología, Facultad de Medicina, Universidad de Antioquia.
References
Joly P, Horvath B, Patsatsi Α, Uzun S, Bech R, Beissert S, et al. Updated S2K guidelines on the management of pemphigus vulgaris and foliaceus initiated by the european academy of dermatology and venereology (EADV). J Eur Acad Dermatol Venereol. septiembre de 2020;34(9):1900-13.
Murrell DF, Peña S, Joly P, Marinovic B, Hashimoto T, Diaz LA, et al. Diagnosis and management of pemphigus: Recommendations of an international panel of experts. J Am Acad Dermatol. marzo de 2020;82(3):575-585.e1.
Schmidt E, Kasperkiewicz M, Joly P. Pemphigus. The Lancet. septiembre de 2019;394(10201):882-94.
Hébert V, Boulard C, Houivet E, Duvert Lehembre S, Borradori L, Della Torre R, et al. Large International Validation of ABSIS and PDAI Pemphigus Severity Scores. Journal of Investigative Dermatology. enero de 2019;139(1):31-7.
Etesami I, Dadkhahfar S, Kalantari Y. Topical care in pemphigus wounds: A systematic review of the literature. Dermatologic Therapy [Internet]. noviembre de 2022 [citado 7 de agosto de 2023];35(11). Disponible en: https://onlinelibrary.wiley.com/doi/10.1111/dth.15808
Grada A, Obagi Z, Phillips T. Management of chronic wounds in patients with pemphigus. CWCMR. agosto de 2019;Volume 6:89-98.
Blackett AV. Managing painful surface wounds. Oncology (Williston Park). julio de 2007;21(8 Suppl):16-9.
Joly P, Maho-Vaillant M, Prost-Squarcioni C, Hebert V, Houivet E, Calbo S, et al. First-line rituximab combined with short-term prednisone versus prednisone alone for the treatment of pemphigus (Ritux 3): a prospective, multicentre, parallel-group, open-label randomised trial. The Lancet. mayo de 2017;389(10083):2031-40.
Shahidi-Dadras M, Karami A, Toosy P, Shafiyan A. Pulse versus oral methylprednisolone therapy in pemphigus vulgaris. Arch Iran Med. enero de 2007;10(1):1-6.
Mignogna MD, Lo Muzio L, Ruoppo E, Fedele S, Lo Russo L, Bucci E. High-dose intravenous ‘pulse’ methylprednisolone in the treatment of severe oropharyngeal pemphigus: a pilot study: High-dose intravenous ‘pulse’ methylprednisolone in the treatment of severe oropharyngeal pemphigus. Journal of Oral Pathology & Medicine. julio de 2002;31(6):339-44.
Löwenberg M, Verhaar AP, van den Brink GR, Hommes DW. Glucocorticoid signaling: a nongenomic mechanism for T-cell immunosuppression. Trends Mol Med. abril de 2007;13(4):158-63.
Lee MS, Yeh YC, Tu YK, Chan TC. Network meta-analysis–based comparison of first-line steroid-sparing adjuvants in the treatment of pemphigus vulgaris and pemphigus foliaceus. Journal of the American Academy of Dermatology. julio de 2021;85(1):176-86.
Chams-Davatchi C, Mortazavizadeh A, Daneshpazhooh M, Davatchi F, Balighi K, Esmaili N, et al. Randomized double blind trial of prednisolone and azathioprine, vs. prednisolone and placebo, in the treatment of pemphigus vulgaris: Azathioprine in pemphigus vulgaris: a randomized controlled trial. Journal of the European Academy of Dermatology and Venereology. octubre de 2012;no-no.
Leis-Dosil VM, Prats-Caelles I. Manejo práctico de inmunosupresores en dermatología. Actas Dermo-Sifiliográficas. enero de 2018;109(1):24-34.
Chavez-Alvarez S, Herz-Ruelas M, Villarreal-Martinez A, Ocampo-Candiani J, Garza-Garza R, Gomez-Flores M. Azathioprine: its uses in dermatology. Anais Brasileiros de Dermatologia. noviembre de 2020;95(6):731-6.
Beissert S, Mimouni D, Kanwar AJ, Solomons N, Kalia V, Anhalt GJ. Treating Pemphigus Vulgaris with Prednisone and Mycophenolate Mofetil: A Multicenter, Randomized, Placebo-Controlled Trial. Journal of Investigative Dermatology. agosto de 2010;130(8):2041-8.
Chams-Davatchi C, Esmaili N, Daneshpazhooh M, Valikhani M, Balighi K, Hallaji Z, et al. Randomized controlled open-label trial of four treatment regimens for pemphigus vulgaris. Journal of the American Academy of Dermatology. octubre de 2007;57(4):622-8.
Martin LK, Werth VP, Villaneuva EV, Murrell DF. A systematic review of randomized controlled trials for pemphigus vulgaris and pemphigus foliaceus. Journal of the American Academy of Dermatology. mayo de 2011;64(5):903-8.
Werth VP, Joly P, Mimouni D, Maverakis E, Caux F, Lehane P, et al. Rituximab versus Mycophenolate Mofetil in Patients with Pemphigus Vulgaris. N Engl J Med. 17 de junio de 2021;384(24):2295-305.
Kridin K, Mruwat N, Ludwig RJ. Association of Rituximab With Risk of Long-term Cardiovascular and Metabolic Outcomes in Patients With Pemphigus. JAMA Dermatol. 1 de enero de 2023;159(1):56.
Kridin K, Mruwat N, Amber KT, Ludwig RJ. Risk of infections in patients with pemphigus treated with rituximab vs. azathioprine or mycophenolate mofetil: a large-scale global cohort study. British Journal of Dermatology. 30 de marzo de 2023;188(4):499-505.
Dong HJ, Ni LN, Sheng GF, Song HL, Xu JZ, Ling Y. Risk of hepatitis B virus (HBV) reactivation in non-Hodgkin lymphoma patients receiving rituximab-chemotherapy: A meta-analysis. Journal of Clinical Virology. julio de 2013;57(3):209-14.
España A, Ornilla E, Panizo C. Rituximab en dermatología. Actas Dermo-Sifiliográficas. junio de 2013;104(5):380-92.
Werth VP, Fivenson D, Pandya AG, Chen D, Rico MJ, Albrecht J, et al. Multicenter randomized, double-blind, placebo-controlled, clinical trial of dapsone as a glucocorticoid-sparing agent in maintenance-phase pemphigus vulgaris. Arch Dermatol. enero de 2008;144(1):25-32.
Chatterjee M, Meru S, Vasudevan B, Deb P, Moorchung N. Pemphigus foliaceus masquerading as IgA pemphigus and responding to dapsone. Indian J Dermatol. noviembre de 2012;57(6):495-7.
Amagai M, Ikeda S, Shimizu H, Iizuka H, Hanada K, Aiba S, et al. A randomized double-blind trial of intravenous immunoglobulin for pemphigus. J Am Acad Dermatol. abril de 2009;60(4):595-603.
S H, E S, M G, Eb B, D Z. Serum levels of autoantibodies to desmoglein 3 in patients with therapy-resistant pemphigus vulgaris successfully treated with adjuvant intravenous immunoglobulins. Acta dermato-venereologica [Internet]. 2004 [citado 9 de agosto de 2023];84(1). Disponible en: https://pubmed-ncbi-nlm-nih-gov.consultaremota.upb.edu.co/15040478/
Green MG, Bystryn JC. Effect of intravenous immunoglobulin therapy on serum levels of IgG1 and IgG4 antidesmoglein 1 and antidesmoglein 3 antibodies in pemphigus vulgaris. Arch Dermatol. diciembre de 2008;144(12):1621-4.
Czernik A, Beutner EH, Bystryn JC. Intravenous immunoglobulin selectively decreases circulating autoantibodies in pemphigus. J Am Acad Dermatol. mayo de 2008;58(5):796-801.
Bystryn JC, Rudolph JL. IVI g TREATMENT OF PEMPHIGUS: how it works and how to use it. J Invest Dermatol. diciembre de 2005;125(6):1093-8.
Sami N, Qureshi A, Ruocco E, Ahmed AR. Corticosteroid-sparing effect of intravenous immunoglobulin therapy in patients with pemphigus vulgaris. Arch Dermatol. septiembre de 2002;138(9):1158-62.
R E, M H. Immunoadsorption in pemphigus. Autoimmunity [Internet]. noviembre de 2006 [citado 9 de agosto de 2023];39(7). Disponible en: https://pubmed-ncbi-nlm-nih-gov.consultaremota.upb.edu.co/17101505/
Ranugha PSS, Kumari R, Kartha LB, Parameswaran S, Thappa DM. Therapeutic plasma exchange as a crisis option in severe pemphigus vulgaris. Indian J Dermatol Venereol Leprol. 2012;78(4):508-10.
Cotterill JA, Barker DJ, Millard LG. Plasma exchange in the treatment of pemphigus vulgaris. Br J Dermatol. febrero de 1978;98(2):243.
Schmidt E, Klinker E, Opitz A, Herzog S, Sitaru C, Goebeler M, et al. Protein A immunoadsorption: a novel and effective adjuvant treatment of severe pemphigus. Br J Dermatol. junio de 2003;148(6):1222-9.
Lüftl M, Stauber A, Mainka A, Klingel R, Schuler G, Hertl M. Successful removal of pathogenic autoantibodies in pemphigus by immunoadsorption with a tryptophan-linked polyvinylalcohol adsorber. Br J Dermatol. septiembre de 2003;149(3):598-605.
Pasricha JS, Khaitan BK, Raman RS, Chandra M. Dexamethasone-cyclophosphamide pulse therapy for pemphigus. Int J Dermatol. diciembre de 1995;34(12):875-82.
Kaur S, Kanwar AJ. Dexamethasone-cyclophosphamide pulse therapy in pemphigus. Int J Dermatol. junio de 1990;29(5):371-4.
Sacchidanand S, Hiremath NC, Natraj HV, Revathi TN, Rani S, Pradeep G, et al. Dexamethasone-cyclophosphamide pulse therapy for autoimmune-vesiculobullous disorders at Victoria hospital, Bangalore. Dermatol Online J. diciembre de 2003;9(5):2.
Kim J, Chan JJ. Cyclophosphamide in dermatology: Cyclophosphamide in dermatology. Australasian Journal of Dermatology. febrero de 2017;58(1):5-17.
Kridin K, Zelber-Sagi S, Bergman R. Pemphigus Vulgaris and Pemphigus Foliaceus: Differences in Epidemiology and Mortality. Acta Derm Venerol. 2017;97(9):1095-9.
Narain U, Kant T, Kant A. Incidence of infections in patients with pemphigus vulgaris. International Journal of Advances in Medicine. 24 de mayo de 2022;9(6):666-9.
Kiran KC, Madhukara J, Abraham A, Muralidharan S. Cutaneous Bacteriological Profile in Patients with Pemphigus. Indian J Dermatol. 2018;63(4):301-4.
Harman KE, Brown D, Exton LS, Groves RW, Hampton PJ, Mohd Mustapa MF, et al. British Association of Dermatologists’ guidelines for the management of pemphigus vulgaris 2017. Br J Dermatol. noviembre de 2017;177(5):1170-201.
BAUM S, ATAR I, COSTER D, DOVRAT S, SOLOMON M, SPRECHER E, et al. Relationship Between Pemphigus Vulgaris Severity and PCR-positive Herpes Simplex Virus. Acta Derm Venereol. 4 de mayo de 2022;102:917.
Nili A, Karimi S, Salehi Farid A, Molhem Azar P, Farimani Z, Shahbazian H, et al. Factors associated with the healing time of pemphigus vulgaris oral lesions: A prospective study. Oral Dis. julio de 2023;29(5):2248-55.
Cohen PR, Paravar T, Lee RA. Epidermal multinucleated giant cells are not always a histopathologic clue to a herpes virus infection: multinucleated epithelial giant cells in the epidermis of lesional skin biopsies from patients with acantholytic dermatoses can histologically mimic a herpes virus infection. Dermatol Pract Concept. octubre de 2014;4(4):21-7.
Konda D, Chandrashekar L, Dhodapkar R, Ganesh RN, Thappa DM. Clinical markers of herpes simplex virus infection in patients with pemphigus vulgaris. J Am Acad Dermatol. marzo de 2023;88(3):587-92.
Iraji F, Faghihi G, Siadat AH. The efficacy of acyclovir in treatment of the pemphigus vulgaris. J Res Med Sci. noviembre de 2013;18(11):976-8.
Pranteda G, Carlesimo M, Bottoni U, Di Napoli A, Muscianese M, Pimpinelli F, et al. Pemphigus vulgaris in a patient with arthritis and uveitis: successful treatment with immunosuppressive therapy and acyclovir. Dermatol Ther. 2014;27(4):215-8.
Daneshpazhooh M, Balighi K, Mahmoudi H, Tavakolpour S, Abedini R, Soori T, et al. Iranian guideline for rituximab therapy in pemphigus patients. Dermatol Ther. septiembre de 2019;32(5):e13016.
Ghadiri K, Vaziri S, Afsharian M, Jahanbaksh A, Mansouri F, Sayad M, et al. Comparison of the accelerated and standard vaccination schedules against hepatitis B in healthcare workers. J Res Med Sci. octubre de 2012;17(10):934-7.
Huang X, Liang X, Zhang J, Su H, Chen Y. Pemphigus during the COVID-19 Epidemic: Infection Risk, Vaccine Responses and Management Strategies. JCM. 8 de julio de 2022;11(14):3968.
How to Cite
Downloads
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Camilo Ruiz, Jennifer Arenas Sepúlveda, Erika Patricia Muñoz Herrera, Jurany Andrea Sánchez Bustamante, Luisa Hernández Tejada, Daniela Astarot Uribe Salazar, José Tomás Peralta Fuentes, Marcos Stivel Munera Patiño, Paula Andrea Aristizabal Diaz, Santiago Beuth Ruiz; Margarita María Velásquez Lopera; Gloria Andrea Vargas Suaza, Claudia Patricia Palacios Isaza, Carlos Eduardo Montealegre Gómez; Oscar Jairo Valencia Ocampo; Manuel Antonio Martínez Gómez, Miguel Mateo Cuervo López, Alberto de Jesús Uribe Correa, Juan David Ruiz Restrepo, Juan Pablo Ospina Gómez, Luis Alfonso Correa Londoño

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |






