Manifestaciones dermatológicas por Covid-19 y su aporte en la comprensión de la enfermedad
DOI:
https://doi.org/10.29176/2590843X.1641Palabras clave:
Cabello, Enfermedad por coronavirus 2019-nCoV, Eritema pernio, Exantema, Fisiopatología, Livedo reticular, Manifestaciones cutáneas, Mucosa oral, Piel, Púrpura, Uñas, Urticaria, VesículaResumen
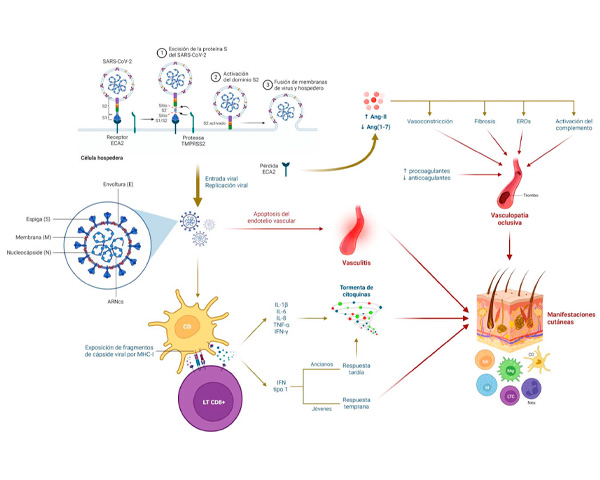
La enfermedad por coronavirus (Covid-19) presenta compromiso multisistémico y hasta en el 20% de los casos puede exhibir signos dermatológicos. Se realiza una revisión narrativa de la literatura acerca de las principales manifestaciones mucocutáneas asociadas a la infección por Covid-19. También se describen brevemente los mecanismos fisiopatológicos y se lleva a cabo una clasificación de las lesiones en maculopapulares, urticariales, vesiculoampollosas, tipo pernio, livedo necróticas, vasculíticas, con compromiso del folículo piloso, ungular u oral. Se presentan sus principales características clínicas, histopatológicas y tratamientos.
Biografía del autor/a
Heliana Botello, Universidad de Caldas: Manizales, Caldas, CO
Médica Dermatóloga, Coordinadora Semillero de Investigación en Dermatología (SIDERM) , Universidad de Caldas.
Adriana Zamudio Barrientos, Universidad de Cartagena: Cartagena, Bolivar, CO
Residente de Tercer año de dermatología, Universidad de Cartagena.
Manuel Eduardo Gahona Naranjo, Pontificia Universidad Javeriana: Bogotá, Cundinamarca, CO
Médico general, Pontificia Universidad Javeriana.
Referencias bibliográficas
Singh H, Kaur H, Singh K, Sen CK. Cutaneous manifestations of COVID-19: A systematic review. Advances in Wound Care. 2021;10(2):51-80. https://doi.org/10.1089/wound.2020.1309
Perlman S. Another Decade, Another Coronavirus. N Engl J Med. 2020;382(8):760-2. https://doi.org/10.1056/nejme2001126
Millán-Oñate J, Rodriguez-Morales AJ, Camacho-Moreno G, Mendoza-Ramírez H. A new emerging zoonotic virus of concern : the 2019 novel Coronavirus (SARS CoV-2 ). Infectio. 2021;24(3):187-92.
Zhou P, Yang X, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270-3. https://doi.org/10.1038/s41586-020-2012-7
Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China. JAMA. 2020;323(13):1239. https://doi.org/10.1001/jama.2020.2648
Guan W, Ni Z, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708-20. https://doi.org/10.1056/nejmoa2002032
Tammaro A, Adebanjo GAR, Parisella FR, Pezzuto A, Rello J. Cutaneous manifestations in COVID-19: the experiences of Barcelona and Rome. J Eur Acad Dermatol Venereol. 2020;34(7):e306-e307. https://doi.org/10.1111/jdv.16530
Fernandez-Nieto D, Ortega-Quijano D, Segurado-Miravalles G, Pindado-Ortega C, Prieto-Barrios M, Jimenez-Cauhe J. Comment on: Cutaneous manifestations in COVID-19: a first perspective. Safety concerns of clinical images and skin biopsies. J Eur Acad Dermatol Venereol. 2020;34(6):e252-e254. https://doi.org/10.1111/jdv.16470
Galván C, Català A, Carretero G, Rodríguez P, Fernández D, Rodríguez A, et al. Classification of the cutaneous manifestations of COVID-19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol. 2020;183(1):71-7. https://doi.org/10.1111/bjd.19163
Ortega-Quijano D, Jimenez-Cauhe J, Selda-Enriquez G, Fernandez-Guarino M, Fernandez-Nieto D. Algorithm for the classification of COVID-19 rashes. J Am Acad Dermatol. 2020;83(2):e103-e104. https://doi.org/10.1016/j.jaad.2020.05.034
Freeman EE, McMahon DE, Lipoff JB, Thiers B, Hruza G, Fox L, et al. The spectrum of COVID-19-associated dermatologic manifestations: An international registry of 716 patients from 31 countries. J Am Acad Dermatol. 2020;83(4):1118-29. https://doi.org/10.1016/j.jaad.2020.06.1016
Carrascosa JM, Morillas V, Bielsa I, Munera-Campos M. Cutaneous Manifestations in the Context of SARS-CoV-2 Infection (COVID-19). Actas Dermo-Sifiliograficas. 2020;111(9):734-43. https://doi.org/10.1016/j.ad.2020.08.002
Pastrian-Soto G, Pastrian-Soto G. Bases Genéticas y Moleculares del COVID-19 (SARS-CoV-2). Mecanismos de Patogénesis y de Respuesta Inmune. Int J Odontostomatol. 2020;14(3):331-7. https://doi.org/10.4067/S0718-381X2020000300331
Magro C, Mulvey JJ, Berlin D, Nuovo G, Salvatore S, Harp J, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. Trans Research. 2020;220:1-13. https://doi.org/10.1016/j.trsl.2020.04.007
Bevacqua R, Perrone S. COVID-19: relación entre enzima convertidora de angiotensina 2, sistema cardiovascular y respuesta inmune del huésped. Insuf Card. 2020;15(2):34-51.
González González F, Cortés Correa C, Peñaranda Contreras E. Manifestaciones cutáneas en pacientes con COVID-19: características clínicas y mecanismos fisiopatológicos postulados. Actas Dermo-Sifiliográficas. 2021;112(4):314-23. https://doi.org/10.1016/J.AD.2020.11.013
Shams S, Rathore SS, Anvekar P, Sondhi M, Kancherla N, Tousif S, et al. Maculopapular skin eruptions associated with Covid-19: A systematic review. Dermatol Ther. 2021;34(2):e14788. https://doi.org/10.1111/DTH.14788
Li M-Y, Li L, Zhang Y, Wang X-S. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Pov. 2020;9(1). https://doi.org/10.1186/S40249-020-00662-X
Xue X, Mi Z, Wang Z, Pang Z, Liu H, Zhang F. High Expression of ACE2 on Keratinocytes Reveals Skin as a Potential Target for SARS-CoV-2. J Invest Dermatol. 2021;141(1):206. https://doi.org/10.1016/J.JID.2020.05.087
Al-Benna S. Gene Expression of Angiotensin-Converting Enzyme 2 Receptor in Skin and the Implications for COVID-19. Adv Skin Wound Care. 2021;34(1):31-5. https://doi.org/10.1097/01.ASW.0000722748.73437.7D
Zhu R, Shi Y, Tan Y, Xiao R. ACE2 Expression on the Keratinocytes and SARS-CoV-2 Percutaneous Transmission: Are they Related? J Invest Dermatol. 2021;141(1):197. https://doi.org/10.1016/J.JID.2020.09.019
Jamshidi P, Hajikhani B, Mirsaeidi M, Vahidnezhad H, Dadashi M, Nasiri MJ. Skin Manifestations in COVID-19 Patients: Are They Indicators for Disease Severity? A Systematic Review. Front Med. 2021;8:634208. https://doi.org/10.3389/FMED.2021.634208
Kubanov AA, Deryabin DG. Skin manifestations in COVID-19 provide a clue for disease’s pathophysiology understanding. J Eur Acad Dermatol Venereol. 2021;35(1):e3-e4. https://doi.org/10.1111/JDV.16902
Zhang Y, Cao W, Jiang W, Xiao M, Li Y, Tang N, et al. Profile of natural anticoagulant, coagulant factor and anti-phospholipid antibody in critically ill COVID-19 patients. J Thromb Thrombolysis. 2020;50(3):580-6. https://doi.org/10.1007/S11239-020-02182-9
Li H, Liu L, Zhang D, Xu J, Dai H, Tang N, et al. SARS-CoV-2 and viral sepsis: observations and hypotheses. Lancet. 2020;395(10235):1517-20. https://doi.org/10.1016/S0140-6736(20)30920-X
Gianotti R, Veraldi S, Recalcati S, Cusini M, Ghislanzoni M, Boggio F, et al. Cutaneous clinico-pathological findings in three covid-19-positive patients observed in the metropolitan area of Milan, Italy. Acta Dermato-Venereologica. 2020;100(8):adv00126. https://doi.org/10.2340/00015555-3490
Campo-Slebi I, Meza-Corso MF, Cárdenas P, Castro-Ayarza JR, González C, Cortés C, et al. COVID-19 in patients with psoriasis: A Latin American case series. JAAD Int. 2021;5:96-7. https://doi.org/10.1016/j.jdin.2021.09.001
Kolivras A, Dehavay F, Delplace D, Feoli F, Meiers I, Milone L, et al. Coronavirus (COVID-19) infection–induced chilblains: A case report with histopathologic findings. JAAD Case Rep. 2020;6(6):489-92. https://doi.org/10.1016/J.JDCR.2020.04.011
Rajan B, Kumar-M P, Bhardwaj A. The trend of cutaneous lesions during COVID-19 pandemic: lessons from a meta-analysis and systematic review. Int J Dermatol. 2020;59(11):1358-70. https://doi.org/10.1111/IJD.15154
Jones VG, Mills M, Suarez D, Hogan C, Yeh D, Segal J, et al. COVID-19 and Kawasaki Disease: Novel Virus and Novel Case. Hosp Pediatr. 2020;10(6):537-40. https://doi.org/10.1542/HPEDS.2020-0123
Mahé A, Birckel E, Krieger S, Merklen C, Bottlaender L. A distinctive skin rash associated with coronavirus disease 2019? J Eur Acad Dermatol Venereol. 2020;34(6):e246-e247. https://doi.org/10.1111/JDV.16471
Sachdeva M, Gianotti R, Shah M, Bradanini L, Tosi D, Veraldi S, et al. Cutaneous manifestations of COVID-19: Report of three cases and a review of literature. J Dermatol Sci. 2020;98(2):75-81. https://doi.org/10.1016/J.JDERMSCI.2020.04.011
Mirza FN, Malik AA, Omer SB, Sethi A. Dermatologic manifestations of COVID-19: a comprehensive systematic review. Int J Dermatol. 2021;60(4):418-50. https://doi.org/10.1111/IJD.15168
Conforti C, Dianzani C, Agozzino M, Giuffrida R, Marangi G, di Meo N, et al. Cutaneous Manifestations in Confirmed COVID-19 Patients: A Systematic Review. Biology. 2020;9(12):1-28. https://doi.org/10.3390/BIOLOGY9120449
Seirafianpour F, Sodagar S, Mohammad AP, Panahi P, Mozafarpoor S, Almasi S, et al. Cutaneous manifestations and considerations in COVID-19 pandemic: A systematic review. Dermatol Ther. 2020;33(6):e13986. https://doi.org/10.1111/DTH.13986
De Masson A, Bouaziz JD, Sulimovic L, Cassius C, Jachiet M, Ionescu M, et al. Chilblains is a common cutaneous finding during the COVID-19 pandemic: A retrospective nationwide study from France. J Am Acad Dermatol. 2020;83(2):667-70. https://doi.org/10.1016/j.jaad.2020.04.161
Hedou M, Carsuzaa F, Chary E, Hainaut E, Cazenave-Roblot F, Masson Regnault M. Comment on ‘Cutaneous manifestations in COVID-19: a first perspective’ by Recalcati S. J Eur Acad Dermatol Venereol. 2020;34(7):e299-e300. https://doi.org/10.1111/jdv.16519
Marzano AV, Genovese G, Fabbrocini G, Pigatto P, Monfrecola G, Piraccini B, et al. Varicella-like exanthem as a specific COVID-19–associated skin manifestation: Multicenter case series of 22 patients. J Am Acad Dermatol. 2020;83(1):280-5. https://doi.org/10.1016/j.jaad.2020.04.044
Askin O, Altunkalem RN, Altinisik DD, Uzuncakmak TK, Tursen U, Kutlubay Z. Cutaneous manifestations in hospitalized patients diagnosed as COVID-19. Dermatol Ther. 2020;33(6). https://doi.org/10.1111/dth.13896
Rubio-Muniz CA, Puerta-Peña M, Falkenhain-López D, Arroyo-Andrés J, Agud-Dios M, Rodriguez-Peralto J, et al. The broad spectrum of dermatological manifestations in COVID-19: clinical and histopathological features learned from a series of 34 cases. J Eur Acad Dermatol Venereol. 2020;34(10):e574-e576. https://doi.org/10.1111/jdv.16734
Méndez Maestro I, Peña Merino L, Udondo González del Tánago B, Aramburu González A, Orbea Sopeña A, Sánchez De Vicente J, et al. Skin manifestations in patients hospitalized with confirmed COVID-19 disease: a cross-sectional study in a tertiary hospital. Int J Dermatol. 2020;59(11):1353-7. https://doi.org/10.1111/ijd.15180
Morey-Olivé M, Espiau M, Mercadal-Hally M, Lera-Carballo E, García-Patos V. Cutaneous manifestations in the current pandemic of coronavirus infection disease (COVID 2019). Ann Pediatr. 2020;92(6):374-5. https://doi.org/10.1016/j.anpede.2020.04.002
Henry D, Ackerman M, Sancelme E, Finon A, Esteve E. Urticarial eruption in COVID-19 infection. J Eur Acad Dermatol Venereol. 2020;34(6):e244-e245. https://doi.org/10.1111/jdv.16472
Rivera-Oyola R, Koschitzky M, Printy R, Liu S, Stanger R, Golant A, et al. Dermatologic findings in 2 patients with COVID-19. JAAD Case Rep. 2020;6(6):537-9. https://doi.org/10.1016/j.jdcr.2020.04.027
van Damme C, Berlingin E, Saussez S, Accaputo O. Acute urticaria with pyrexia as the first manifestations of a COVID-19 infection. J Eur Acad Dermatol Venereol. 2020;34(7):e300-e301. https://doi.org/10.1111/jdv.16523
Lu S, Lin J, Zhang Z, Xiao L, Jiang Z, Chen J, et al. Alert for non-respiratory symptoms of coronavirus disease 2019 patients in epidemic period: A case report of familial cluster with three asymptomatic COVID-19 patients. J Med Virol. 2021;93(1):518-21. https://doi.org/10.1002/jmv.25776
Fernandez-Nieto D, Ortega-Quijano D, Jimenez-Cauhe J, Burgos-Blasco P, De Perosanz-Lobo D, Suarez-Valle A, et al. Clinical and histological characterization of vesicular COVID-19 rashes: a prospective study in a tertiary care hospital. Clin Exp Dermatol. 2020;45(7):872-5. https://doi.org/10.1111/ced.14277
Mahé A, Birckel E, Merklen C, Lefèbvre P, Hannedouche C, Jost M, et al. Histology of skin lesions establishes that the vesicular rash associated with COVID-19 is not ‘varicella-like’. J Eur Acad Dermatol Venereol. 2020;34(10):e559-e561. https://doi.org/10.1111/jdv.16706
Keshavarzi A, Mohammadi AA, Ayaz M, Javanmardi F, Hoghoughi M, Yeganeh B, et al. Cutaneous Vesicular of COVID-19 in Two Burn Patients. World J Plast Surg. 2020;9(3):331-8. https://doi.org/10.29252/wjps.9.3.331
García-Gil MF, Monte Serrano J, García García M, Barra Borao V, Matovelle Ochoa C, Ramirez-Lluch M, et al. Acral purpuric lesions associated with coagulation disorders during the COVID-19 pandemic. Int J Dermatol. 2020;59(9):1151-2. https://doi.org/10.1111/ijd.15041
Bouaziz JD, Duong TA, Jachiet M, Velter C, Lestang P, Cassius C, et al. Vascular skin symptoms in COVID-19: a French observational study. J Eur Acad Dermatol Venereol. 2020;34(9):e451-e452. https://doi.org/10.1111/jdv.16544
Recalcati S, Barbagallo T, Frasin LA, Prestinari F, Cogliardi A, Provero M, et al. Acral cutaneous lesions in the time of COVID-19. J Eur Acad Dermatol Venereol. 2020;34(8):e346-e347. https://doi.org/10.1111/jdv.16533
Alramthan A, Aldaraji W. Two cases of COVID-19 presenting with a clinical picture resembling chilblains: first report from the Middle East. Clin Exp Dermatol. 2020;45(6):746-8. https://doi.org/10.1111/ced.14243
Pavone P, Marino S, Marino L, Cacciaguerra G, Guarneri C, Nunnari G, et al. Chilblains-like lesions and SARS-CoV-2 in children: An overview in therapeutic approach. Dermatol Ther. 2021;34(1):2-6. https://doi.org/10.1111/dth.14502
Landa N, Mendieta-Eckert M, Fonda-Pascual P, Aguirre T. Chilblain-like lesions on feet and hands during the COVID-19 Pandemic. Int J Dermatol. 2020;59(6):739-43. https://doi.org/10.1111/ijd.14937
Docampo-Simón A, Sánchez-Pujol MJ, Juan-Carpena G, Palazón-Cabanes J, Vergara-De Caso E, Berbegal L, et al. Are chilblain-like acral skin lesions really indicative of COVID-19? A prospective study and literature review. J Eur Acad Dermatol Venereol. 2020;34(9):e445-e447. https://doi.org/10.1111/jdv.16665
Cappel M, Cappel J, Wetter D. Pernio (Chilblains), SARS-CoV-2, and COVID Toes Unified Through Cutaneous and Systemic Mechanisms. Mayo Clin Proc. 2020;96(4):989-1005. https://doi.org/10.1016/j.mayocp.2021.01.009
Kluger N. Livedoid vasculopathy. Forum for N Dermato-Venerol. 2018;23(1):3-5. https://doi.org/10.5005/jp/books/13043_34
Gottlieb M, Long B. Dermatologic manifestations and complications of COVID-19. Am J Emerg Med. 2020;38(9):1715-21. https://doi.org/10.1016/j.ajem.2020.06.011
Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemostasis. 2020;18(4):844-7. https://doi.org/10.1111/jth.14768
Naderi-Azad S, Vender R. Lessons From the First Wave of the Pandemic: Skin Features of COVID-19 Can Be Divided Into Inflammatory and Vascular Patterns. J Cut Med Surg. 2021;25(2):169-76. https://doi.org/10.1177/1203475420972343
Wambier CG, Vaño-Galván S, McCoy J, Shapiro J, Pérez B, Goren A, et al. Androgenetic alopecia present in the majority of patients hospitalized with COVID-19: The “Gabrin sign.” J Am Acad Dermatol. 2020;83(2):680-2. https://doi.org/10.1016/j.jaad.2020.05.079
Müller Ramos P, Ianhez M, Amante Miot H. Alopecia and grey hair are associated with COVID-19 Severity. Exp Dermatol. 2020;29(12):1250-2. https://doi.org/10.1111/exd.14220
Wambier C, Goren A. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection is likely to be androgen mediated. J Am Acad Dermatol. 2020;83(1):308-9. https://doi.org/10.1016/j.jaad.2020.04.032
Berbert Ferreira S, Gavazzoni Dias MFR, Berbert Ferreira R, Neves Neto AC, Trüeb RM, Lupi O. Rapidly progressive alopecia areata totalis in a COVID-19 patient, unresponsive to tofacitinib. J Eur Acad Dermatol Venereol. 2021;35(7):e411-e412. https://doi.org/10.1111/jdv.17170
Rizzetto G, Diotallevi F, Campanati A, Radi G, Bianchelli T, Molinelli E, et al. Telogen effluvium related to post severe Sars-Cov-2 infection: Clinical aspects and our management experience. Dermatol Ther. 2021;34(1):1-6. https://doi.org/10.1111/dth.14547
Shanshal M. COVID-19 related anagen effluvium. J Dermatol Treat. 2020;0(0):1-2. https://doi.org/10.1080/09546634.2020.1792400
Moreno-Arrones OM, Lobato-Berezo A, Gomez-Zubiaur A, Arias-Santiago S, Saceda-Corralo D, Bernardez-Guerra C, et al. SARS-CoV-2-induced telogen effluvium: a multicentric study. J Eur Acad Dermatol Venereol. 2021;35(3):e181-e183. https://doi.org/10.1111/jdv.17045
Natalello G, Luca G De, Gigante L, Campochiaro C, De Lorenzis E, Verardi L, et al. Nailfold capillaroscopy findings in patients with coronavirus disease 2019: Broadening the spectrum of COVID-19 microvascular involvement. Microvasc Res. 2021;133:104071. https://doi.org/10.1016/j.mvr.2020.104071
Alobaida S, Lam JM. Beau lines associated with COVID-19. CMAJ. 2020;192(36):E1040. https://doi.org/10.1503/cmaj.201619
Ide S, Morioka S, Inada M, Ohmagari N. Beau’s lines and leukonychia in a COVID-19 patient. Int Med. 2020;59(24):3259. https://doi.org/10.2169/internalmedicine.6112-20
Aslan Kayıran M, Cebeci F, Erdemir VA, Aksoy H, Akdeniz N, Gürel MS. Fluorescence of nails and hair on Wood’s lamp examination in Covid pandemic; undefined effect of Favipiravir in humans. Dermatol Ther. 2021;34(1):1-4. https://doi.org/10.1111/dth.14740
Dziedzic A, Wojtyczka R. The impact of coronavirus infectious disease 19 (COVID-19) on oral health. Oral Dis. 2021;27(S3):703-6. https://doi.org/10.1111/odi.13359
Paradowska-Stolarz AM. Oral manifestations of covid-19: Brief review. Dental Med Problems. 2021;58(1):123-6. https://doi.org/10.17219/dmp/131989
Amorim dos Santos J, Normando AGC, Carvalho da Silva RL, Cembranel A, Santos A, Silva E, et al. Oral mucosal lesions in a COVID-19 patient: New signs or secondary manifestations? International J Infect Dis. 2020;97:326-8. https://doi.org/10.1016/j.ijid.2020.06.012
Nuno-Gonzalez A, Martin-Carrillo P, Magaletsky K, Rios M, Herranz Mañas C, Artigas Almazan J, et al. Prevalence of mucocutaneous manifestations in 666 patients with COVID-19 in a field hospital in S pain: oral and palmoplantar findings. Br J Dermatol. 2021;184(1):184-5. https://doi.org/10.1111/bjd.19564
Amorim dos Santos J, Normando AGC, Carvalho da Silva RL, Acevedo A, De Luca Canto G, Sugaya N, et al. Oral Manifestations in Patients with COVID-19: A Living Systematic Review. J Dental Res. 2021;100(2):141-54. https://doi.org/10.1177/0022034520957289
Cómo citar
Descargas
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2023 Revista de la Asociación Colombiana de Dermatología y Cirugía Dermatológica

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-CompartirIgual 4.0.

| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |






