Trends in dermatology: contributions from a study group
DOI:
https://doi.org/10.29176/2590843X.1399Keywords:
Melasma, vaginal laser, Vitiligo, atopic dermatitis, cellulite, acne, pigmentary disorders, cannabinoids, dermatoscopy.Abstract
Keeping ourselves up to date with current professional practices is beneficial for our patients, other colleagues, and for our own sake. There are numerous sources of information, however, we must be very careful when reading news or communications about new diagnosis methods, prevention, or, especially, treatment of different skin conditions and diseases. With this in mind, we have analyzed new or controversial topics and reviewed the corresponding literature. To contribute to our colleagues’ continuous development, we present a short summary of cutting-edge subjects that include melasma, vaginal laser, vitiligo, atopic dermatitis, cellulite, acne, pigmentary defects, use of cannabinoids in dermatology, and dermoscopy.
Author Biographies
Adriana R. Cruz
Dermatólogos, Universidad del Valle, Cali, Colombia.
Johanna Luna
Dermatólogos, Universidad del Valle, Cali, Colombia.
Natalia Montoya
Dermatólogos, Universidad del Valle, Cali, Colombia.
María I. Barona
Dermatólogos, Universidad del Valle, Cali, Colombia.
Natalia Vargas
Dermatólogos, Universidad del Valle, Cali, Colombia.
Nathalie Quiroz
Dermatólogos, Universidad del Valle, Cali, Colombia.
Luis F. Balcázar
Dermatólogos, Universidad del Valle, Cali, Colombia.
Doralda Castro
Dermatólogos, Universidad del Valle, Cali, Colombia.
Víctor Benítez
Dermatólogos, Universidad del Valle, Cali, Colombia.
Sara M. Lozada
Dermatólogos, Universidad del Valle, Cali, Colombia.
Juana López
Dermatólogos, Universidad del Valle, Cali, Colombia.
María I. Moreno
Dermatólogos, Universidad del Valle, Cali, Colombia.
Ricardo Rueda
Dermatólogos, Universidad del Valle, Cali, Colombia.
David Arias
Dermatólogos, Universidad del Valle, Cali, Colombia.
References
Bala HR, Lee S, Wong C, Pandya AG, Rodrigues M. Oral tranexamic acid for the treatment of melasma: a review. Dermatol Surg. 2018; 44(6): 814-825.
https://doi.org/10.1097/DSS.0000000000001518
Kim HJ, Moon SH, Cho SH, Lee JD, Sung Kim H. Efficacy and safety of tranexamic acid in melasma: a meta-analysis and systematic review. Acta Derm Venereol. 2017; 97(6-7): 776-781.
https://doi.org/10.2340/00015555-2668
Del Rosario E, Florez-Pollack S, Zapata Jr L, Hernandez K, Tovar-Garza A, Rodrigues M, et al. Randomized, placebo-controlled, double-blind study of oral tranexamic acid in the treatment of moderate-to-severe melasma. J Am Acad Dermatol. 2018; 78(2): 363-369.
https://doi.org/10.1016/j.jaad.2017.09.053
Sharma R, Mahajan VK, Mehta KS, Chauhan PS, Rawat R, Shiny TN. Therapeutic efficacy and safety of oral tranexamic acid and that of tranexamic acid local infiltration with microinjections in patients with melasma: a comparative study. Clin Exp Dermatol. 2017; 42(7): 728-734.
https://doi.org/10.1111/ced.13164
Wang JV, Jhawar N, Saedi N. Tranexamic Acid for Melasma: Evaluating the Various Formulations. J Clinical Aesthetic Dermatol. 2019; 12(8): E73-E74.
Tadir Y, Gaspar A, Lev-Sagie A, Alexiades M, Alinsod R, Bader A, et al. Light and energy based therapeutics for genitourinary syndrome of menopause: consensus and controversies. Lasers Surg Med. 2017; 49(2):137-159.
https://doi.org/10.1002/lsm.22637
González Isaza P, Jaguszewska K, Cardona JL, Lukaszuk M. Long-term effect of thermoablative fractional CO2 laser treatment as a novel approach to urinary incontinence management in women with genitourinary syndrome of menopause. Int Urogynecol J. 2018; 29(2): 211-215.
https://doi.org/10.1007/s00192-017-3352-1
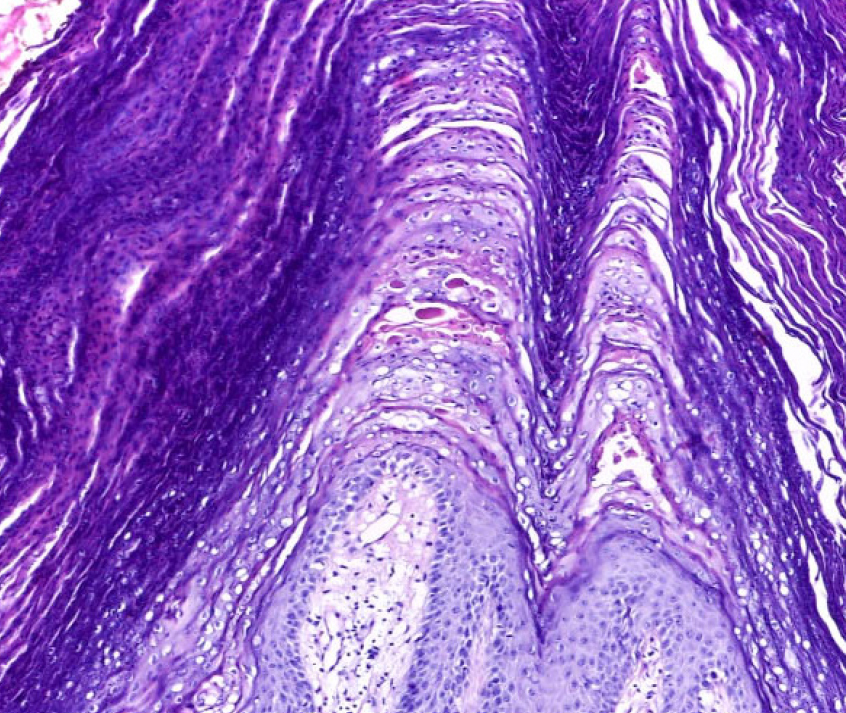
Zerbinati N, Serati M, Origoni M, Candiani M, Lannitti T. Microscopic and ultrastructural modifications of postmenopausal atrophic vaginal mucosa after fractional carbon dioxide laser treatment. Lasers Med Sci. 2015; 30(1): 429-436.
https://doi.org/10.1007/s10103-014-1677-2
Sokol ER, Karram M. An assessment of the safety and efficacy of a fractional CO2 laser system for the treatment of vulvovaginal atrophy. Menopause. 2016; 23(10): 1102-1107.
https://doi.org/10.1097/GME.0000000000000700
Agarwal P, Rashighi M, Essien KI, Richmond J, Randall L, Pazoki-Toroudi H, et al. Simvastatin prevents and reverses depigmentation in a mouse model of vitiligo. J Invest Dermatol. 2015; 135(4): 1080-1088.
https://doi.org/10.1038/jid.2014.529
Vanderweil SG, Amano S, Ko WC, Richmond J, Kelley M, Makredes Senna M, et al. A double-blind, placebo-controlled, phase-II clinical trial to evaluate oral simvastatin as a treatment for vitiligo. J Am Acad Dermatol. 2017; 76(1):150-151.
https://doi.org/10.1016/j.jaad.2016.06.015
Iraji F, Banihashemi SH, Faghihi G, Shahmorad Z, Tajmirriahi N, Bokaie Jazi S. A comparison of betamethasone valerate 0.1% cream twice daily plus oral simvastatin versus betamethasone valerate 0.1% cream alone in the treatment of vitiligo patients. Adv Biomed Res. 2017; 6:34.
https://doi.org/10.4103/2277-9175.203159
Armario-Hita JC, Pereyra-Rodriguez J, Silvestre JF, Ruiz -Villaverde R, Valero A, Izu-Belloso R, et al. Treatment of moderate-to-severe Atopic dermatitis with dupilumab in real clinical practice. A multicentre, retrospective case series. B J Dermatol. 2019: 181(5): 1072-1074
https://doi.org/10.1111/bjd.18041
Seegräber M, Srour J, Walter A, Knop M, Wollenberg A. Dupilumab for treatment of atopic dermatitis. Expert Rev Clin Pharmacol. 2018; 11(5): 467- 474.
https://doi.org/10.1080/17512433.2018.1449642
Gooderham MJ, Hong HC, Eshtiaghi P, Papp K. Dupilumab: A review of its use in the treatment of atopic dermatitis. J Am Acad Dermatol. 2018; 78(3): S28-S36.
https://doi.org/10.1016/j.jaad.2017.12.022
Pérez Atamoros FM, Alcalá Pérez D, Asz Sigall D, Ávila Romay A, Barba Gastelum J , de la Peña Salcedo J. Evidence-based treatment for gynoid lipodystrophy: A review of the recent literature. J Cosmet Dermatology. 2018; 17(6):977-983.
https://doi.org/10.1111/jocd.12555
Zerini I, Sisti A, Cuomo R, Ciappi S, Russo F, Brandi C,et al. Cellulite treatment: a comprehensive literature review. J Cosmet Dermatol. 2015; 14(3): 224-240.
https://doi.org/10.1111/jocd.12154
Rossi AM, Katz BE. A modern approach to the treatment of cellulite. Dermatol Clin, 2014; 32(1): 51-59.
https://doi.org/10.1016/j.det.2013.09.005
Zouboulis CC, Dessinioti C, Tsatsou F, Gollnick H. Anti-acne drugs in phase 1 and 2 clinical trials. Expert Opin Invest Drugs. 2017; 26(7): 813-823.
https://doi.org/10.1080/13543784.2017.1337745
Tan J, Thiboutot D, Popp G, Gooderham M, Lynde C, Del Rosso J, et al. Randomized phase 3 evaluation of trifarotene 50 μg/g cream treatment of moderate facial and truncal acne. J Am Acad Dermatol. 2019; 80(6): 1691-1699.
https://doi.org/10.1016/j.jaad.2019.02.044
Trifu V, Tiplica GS, Naumescu E, Zalupca L, Moro L, Celasco G. Cortexolone 17α-propionate 1% cream, a new potent antiandrogen for topical treatment of acne vulgaris. A pilot randomized, doubleblind comparative study vs. placebo and tretinoin 0· 05% cream. Br J Dermatol. 2011; 165(1):177-183.
https://doi.org/10.1111/j.1365-2133.2011.10332.x
Videira IF, Moura DF, Magina S. Mechanisms regulating melanogenesis. An Bras Dermatol. 2013; 88(1): 76-83.
https://doi.org/10.1590/S0365-05962013000100009
D'Mello SA, Finlay GJ, Baguley BC, Askarian-Amiri M. Signaling pathways in melanogenesis. Int J Mol Sci. 2016; 17(7):1144
https://doi.org/10.3390/ijms17071144
Yuan XH, Jin ZH. Paracrine regulation of melanogenesis. Br J Dermatol. 2018; 178(3): 632-639.
https://doi.org/10.1111/bjd.15651
Eagleston LRM, Kalani NK, Patel RR, Flaten H, Dunnick C, DellaValle R. Cannabinoids in dermatology: A scoping review. Dermatol Online J. 2018; 24(6)
Moya AI, Ruiz-Rodríguez R. Eficacia y seguridad de los cannabinoides tópicos en dermatología. Piel. 2019; 34(5): 313-315.
https://doi.org/10.1016/j.piel.2018.07.011
Caterina MJ. TRP channel cannabinoid receptors in skin sensation, homeostasis, and inflammation. ACS Chem Neurosci. 2014: 5(11): 1107-1116.
https://doi.org/10.1021/cn5000919
Yélamos O, Braun RP, Liopyris K, Wolner Z, Kerl K, Gerami P,et al. Dermoscopy and dermatopathology correlates of cutaneous neoplasms. J Am Acad Dermatol. 2019; 80(2): 341-363.
https://doi.org/10.1016/j.jaad.2018.07.073
Lallas A, Apalla Z, Ioannides D, Lazaridou E, Kyrgidis A, Broganelli P, et al. Update on dermoscopy of Spitz/Reed naevi and management guidelines by the International Dermoscopy Society. Br J Dermatol. 2017; 177(3): 645-655.
https://doi.org/10.1111/bjd.15339
Yélamos O, Navarrete-Dechent C, Marchetti MA, Rogers T, Apalla Z, Bahadoran P, et al. Clinical and dermoscopic features of cutaneous BAP1- inactivated melanocytic tumors: Results of a multicenter case-control study by the International Dermoscopy Society. J Am Acad Dermatol. 2019; 80(6):1585-1593.
How to Cite
Downloads
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2019 Revista de la Asociación Colombiana de Dermatología y Cirugía Dermatológica

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |






