Hidradenitis Suppurativa, an update. Part II: diagnosis, classification and treatment.
DOI:
https://doi.org/10.29176/2590843X.1760Keywords:
Hidradenitis suppurativa, acne inversa, diagnosis, clasification, Ultrasonography, treatmentAbstract
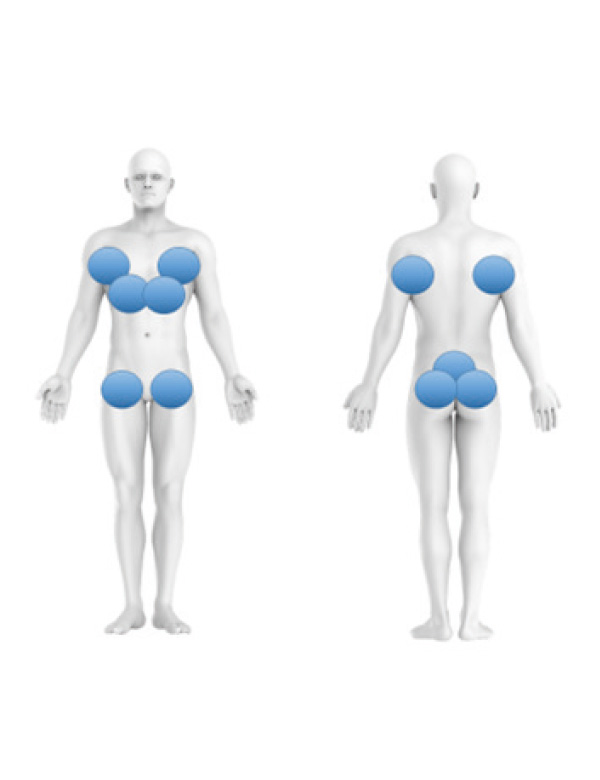
Background: Hidradenitis suppurativa (HS) is a chronic inflammatory skin disorder that involves infundibulofollicular dysfunction and abnormal immune response. It has a peak incidence between the second and third decades of life and clinically presents as painful, chronic, and recurrent suppurative lesions in the intertriginous areas, which evolve into sinuous tracts and deforming scar bands with a remarkable impact on quality of life. This article is a comprehensive review of the state of the art of HS. This second part includes diagnosis, classification, and treatment.
Materials and methods: For this narrative review, a complete literature search was carried out in 3 databases (Pubmed, Science Direct, EMBASE), from 2001 to 2022, including articles published in English and Spanish.
Results: 67 articles published from 2001 to 2022 were included and reviewed in full text.
Conclusion: HS is a complex disease, assessing the severity of the disease clinically and by ultrasonography is essential. The Hurley scale and the modified Sartorious scale are the most used, but new scales are emerging that are useful for assessing patients with this pathology and help define the choice of different therapeutic options
Author Biographies
Juan Guillermo Pabón, Clínica de Marly. Bojanini Health and Skin Experts, Bogotá.
Médico dermatólogo, Clínica de Marly. Bojanini Health and Skin Experts, Bogotá.
Ricardo Flaminio Rojas, Centro Médico Fundación Oftalmológica de Santander (FOSCAL)
Médico dermatólogo, Dermahair Center. Centro Médico Fundación Oftalmológica de Santander (FOSCAL), Floridablanca.
María Isabel Barona, Clínica Imbanaco, Cali.
Médica dermatóloga, Clínica Imbanaco, Cali.
Beatriz Orozco, Independiente
Médico dermatólogo, miembro de la Asociación Colombiana de Dermatología y Cirugía Dermatológica.
Sol Beatriz Jiménez, Universidad CES, Medellín.
Médica dermatóloga, Universidad CES, Medellín.
Esperanza Meléndez, Independiente
Médico dermatólogo, miembro de la Asociación Colombiana de Dermatología y Cirugía Dermatológica, Barranquilla.
Adriana Motta, Universidad El Bosque, Bogotá.
Médica dermatóloga. Directora, Posgrado de Dermatología, Universidad El Bosque, Bogotá.
Lili Johana Rueda, Universidad El Bosque, Bogotá.
Médica dermatóloga. Magíster en Epidemiología. Docente, Posgrado de Dermatología, Universidad El Bosque, Bogotá.
Claudia González, Independiente
Médica radióloga.
Viviana Ibagón, Clínica de Marly, Bogotá.
Médica dermatóloga, Clínica de Marly, Bogotá.
Jessica Vallejo, Independiente
Médico dermatólogo, miembro de la Asociación Colombiana de Dermatología y Cirugía Dermatológica, Bogotá.
Beatriz Armand, Independiente
Médico dermatólogo, miembro de la Asociación Colombiana de Dermatología y Cirugía Dermatológica, Bogotá.
María del Pilar Avellaneda, Independiente
Médico dermatólogo, miembro de la Asociación Colombiana de Dermatología y Cirugía Dermatológica, Bogotá.
Edwin Bendek, Independiente
Médico dermatólogo, miembro de la Asociación Colombiana de Dermatología y Cirugía Dermatológica, Bogotá.
Carlos Montealegre, Universidad de Antioquia, Medellín, Colombia.
Médico dermatólogo. Docente, Posgrado de Dermatología, Universidad de Antioquia, Medellín.
Natalia Velásquez, Universidad CES, Medellín.
Médico dermatólogo. Docente, Posgrado de Dermatología, Universidad CES, Medellín.
Lina Quiroz, Universidad CES, Medellín.
Médico dermatólogo. Docente, Posgrado de Dermatología, Universidad CES, Medellín.
Claudia Uribe, Universidad CES, Medellín.
Médico dermatólogo. Docente, Posgrado de Dermatología, Universidad CES, Medellín.
Cristina Lotero, Universidad CES, Medellín.
Médico dermatólogo. Docente, Posgrado de Dermatología, Universidad CES, Medellín
Diego Espinosa, Universidad CES, Medellín.
Médico dermatólogo. Docente, Posgrado de Dermatología, Universidad CES, Medellín
Jaime Rengifo, Universidad Pontificia Bolivariana, Medellín
Médico dermatólogo. Docente, Posgrado de Dermatología, Universidad Pontificia Bolivariana, Medellín
Rodrigo Nuñez, Universidad Pontificia Bolivariana, Medellín.
Médico dermatólogo. Docente, Posgrado de Dermatología, Universidad Pontificia Bolivariana, Medellín.
References
Goldburg SR, Strober BE PM. Hidradenitis suppurativa. Epidemiology, clinical presentation, and pathogenesis. J Am Acad Dermatol. 2020;82(5):1045-1058. doi:10.1016/j.jaad.2019.08.090
Cabrera-Salom C, Sandoval L, Bulla F. Hidradenitis suppurativa. Piel. 2019;34(7):408-416. doi:10.1016/j.piel.2018.09.002
Martorell FG-M et al. Actualización en hidradenitis supurativa (I): epidemiología, aspectos clínicos y definición de severidad de la enfermedad. Actas Dermosifiliogr. 2015;106(9):703-715.
K. Sellhayer, D K. “Hidradenitis Suppurativa” Is Acne Inversa! An Appeal to (Finally) Abandon a Misnomer. Int J dermatology. 2005;44(7):535-540.
GBE J. Clinical Practice. Hidradenitis Suppurativa. N Engl J Med. 2012;366(2):158-164.
Arantòn Areosa L, Palomar LLatas F RPJ. Formación dermatológica en hidradenitis supurativa o acné inversa. Enferm Dermatol. 2017;11(31):11-21.
Achenbach RE GC. Hidradenitis supurativa. Rev argent Dermatol. 2013;94(4):6-10.
Thorlacius L. Severity staging of hidradenitis suppurativa: is Hurley classification the answer? Br J Dermatol. 2019;181(2):243-244.
Ovadja ZN, Schuit MM, vanderHorst CMAM LO. Inter-andintrarater reliability of Hurley staging for hidradenitis suppurativa. Br J Dermatol. 2019;181(2):344-349.
Sartorius K, Killasli H, Heilborn J, Jemec GB, Lapins J EL. Interobserver variability of clinical scores in hidradenitis suppurativa is low. Br J Dermatol. 2010;162(6):1261-1268.
Hessam S, Scholl L, Sand M et al. A novel severity assessment scoring sistem for hidradenitis suppurativa. JAMA Dermatol. 2018;154(3):330-335.
Hartrick CT et al. The Numeric Rating Scale for Clinical Pain Measurement: A Ratio Measure? Pain Pr. 2003;3(4):310-316.
Molina Leyva A. Importancia de las medidas de gravedad objetiva y subjetiva en la evaluación clínica del paciente con hidradenitis supurativa. Piel. 2019;34(4):199-201.
Wolkenstein P, Loundou A, Barrau K et al. Quality of life impairment in hidradenitis suppurativa: a study of 61cases. J Am Acad Dermatol. 2007;56(4):621-623.
van Straalen K, Ingram J, Augustin M, Zouboulis C. New treatments and new assessment instruments for Hidradenitis suppurativa. Experimental Dermatoly. 2022;31(1):33-39.
Chiricozzi A, Faleri S, Franceschini C, Caro RD, Chimenti S BL. AISI: A New Disease Severity Assessment Tool for Hidradenitis Suppurativa. Wounds. 2015;27(10):258-264.
Thorlacius L, Garg A, Ingram JR et al. Towards global consensus on core outcomes for hidradenitis suppurativa research: an update from the HISTORIC consensus meetings I and II. Br J Dermatol. 2018;178(3):715-721.
Alfagame F, Wortsman X, Catalano o, Roustan G, Crisan M, Crisan D, gaitini E BR. European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) Position Statement on Dermatologic Ultrasound. Ultrasound Med. 2016;35(3):577-580.
González C. Ecografía de lesiones dermatológicas. Rev Colomb Radiol. 2014;25(3):4006-4014.
González C. Ultrasonido de alta resolución en enfermedades benignas de la piel. Rev Asoc Colom Dermatol. 2018;26(4):4230-4239.
Wortsman X. Imaging of Hidradenitis Suppurativa. Dermatol Clin. 2016;34(1):59-68.
Martorell A SPJ. Ultrasound examination of hidradenitis suppurativa. Actas Dermosifiliogr. 2015;106(suppl 1):49-59.
Wortsman X JG. A 3D ultrasound study of sinus tract formation in hidradenitis suppurativa. Dermatol Online J. 2013;19(6):18564.
Napolitano M, Calzavara P, Zanca A, Biacho L, Caposiena R OA et all. Comparison of clinical and ultrasound scores in patients with hidradenitis suppurativa: results from an Italian ultrasound working group. Eur Acad Dermatol Venereol. 2019;33(2):e84-e87.
Martorell F. Alfageme Roldán E. Vilarrasa Rull R. Ruiz‐Villaverde J. Romaní De Gabriel F. García Martínez D. Vidal Sarro M. Velasco Pastor C. Ciudad Blanco J.M. Segura Palacios A.I. Rodríguez Bandera J.C. Pascual Ramírez C. Sancho Sánchez N. Michelena. Ultrasound as a diagnostic and management tool in hidradenitis suppurativa patients: a multicentre study. J Eur Acad Dermatol Venereol. 2019;33(11):2137-2142.
Wortsman X, Alfagame F, Roustan G, Arias-San- tiago S, Martorell A, Catalano O et al. Guidelines for Performing Dermatologic Ultrasound Examinations by the DERMUS Group. J Ultrasound Med. 2016;35(3):577-580.
González C. Hidradenitis supurativa. Descripcion de los hallazgos ecográficos en un centro de referencia en Bogota, Colombia. Rev Asoc Colomb Dermatol. 2020;28(3):240-249.
Martorell A, Worstman X, Alfagame F, Roustan G, Arias-Santiago S, Catalano O, Scotto di Santolo M, Zarchi K, Bouer M, Gattini D, Gonzalez C, Bard R, Garcia -Martínez MA. Ultrasound Evaluation as a Complementary Test in Hidradenitis Suppurativa: Proposal a Standarize report. Dermatol Surg. 2017;43(8):1065-1073.
Wortsman X, Calderon P CA. Seventy-MHz Ultrasound Detection of Early Signs Linked to the Severity, Patterns of Keratin Fragmentation, and Mechanisms of Generation of Collections and Tunnels in Hidradenitis Suppurativa. J Ultrasound Med. 2020;39(5):845-857.
Wortsman X. Dermatologic Ultrasound with clinical and Histologic Correlation. In: Inflammatory Diseases of the Skin. ; 2013:73-118.
Worstman X, Castro A FA. Color Doppler ultrasound assessment of morphology and types of fistulous tracts in hidradenitis suppurative (HS). J Am Acad Dermatol. 2016;75(4):760-767.
Alfagame F. Ecografía de la hidradenitis supurativa. In: Ecografía En Dermatología y Dermoestética ; 2017:57-62.
Wortsman X JG. Real-time compound imaging ultrasound of hidradenitis suppurativa. Dermatol Surg. 2007;33(11):1340-1342.
Saunte DML, Jemec GBE. Hidradenitis Suppurativa: Advances in Diagnosis and Treatment. JAMA. 2017;318(20):2019-2032.
Alikhan A et al. North American clinical management guidelines for hidradenitis suppurativa: A publication from the United States and Canadian Hidradenitis Suppurativa Foundations. Part II: Topical, intralesional, and systemic medical management. JAAD. 2019;81(1):91–101.
Nesbitt E, Clements S, Driscoll M. A concise clinician’s guide to therapy for hidradenitis suppurativa. Int J Womens Dermatol. 2020;6(2):80-84.
Alavi A, Kirsner R. Local wound care and topical management of hidradenitis suppurativa. J Am Acad Dermatol. 2015;73:S55-61
Zouboulis CC, Desai N, Emtestam L, Hunger RE, Ioannides D, Juhász I, Lapins J, Matusiak L, Prens EP, Revuz J, Schneider-Burrus S, Szepietowski JC, van der Zee HH, Jemec GB. European S1 guideline for the treatment of hidradenitis suppurativa/acne inversa. J Eur Acad Dermatol Venereol. 2015 Apr;29(4):619-44. doi: 10.1111/jdv.12966. Epub 2015 Jan 30. PMID: 25640693.
Jørgensen AR, Yao Y, Thomsen SF, Ring HC. Treatment of hidradenitis suppurativa with tetracycline, doxycycline, or lymecycline: a prospective study. Int J Dermatol. 2021 Jul;60(7):785-791. doi: 10.1111/ijd.15459. Epub 2021 Mar 4. PMID: 33660281.
An JH, Moon SJ, Shin JU, Kim DH, Yoon MS, Lee HJ. Clindamycin Mono-Therapy of Hidradenitis Suppurativa Patients: A Single-Center Retrospective Study. Ann Dermatol. 2021 Dec;33(6):515-521. doi: 10.5021/ad.2021.33.6.515. Epub 2021 Nov 4. PMID: 34858002; PMCID: PMC8577909.
Gener G, Canoui-Poitrine F, Revuz JE, Faye O, Poli F, Gabison G, Pouget F, Viallette C, Wolkenstein P, Bastuji-Garin S. Combination therapy with clindamycin and rifampicin for hidradenitis suppurativa: a series of 116 consecutive patients. Dermatology. 2009;219(2):148-54. doi: 10.1159/000228334. Epub 2009 Jul 8. PMID: 19590173.
Mendonça CO, Griffiths CE. Clindamycin and rifampicin combination therapy for hidradenitis suppurativa. Br J Dermatol. 2006 May;154(5):977-8. doi: 10.1111/j.1365-2133.2006.07155.x. PMID: 16634904.
Van der Zee HH, Boer J, Prens EP, Jemec GB. The effect of combined treatment with oral clindamycin and oral rifampicin in patients with hidradenitis suppurativa. Dermatology. 2009;219(2):143-7. doi: 10.1159/000228337. Epub 2009 Jul 8. PMID: 19590174.
Mendes-Bastos P, Macedo R, Duarte R. Treatment of hidradenitis suppurativa with rifampicin: have we forgotten tuberculosis? Br J Dermatol. 2017 Oct;177(4):e150-e151. doi: 10.1111/bjd.15500. Epub 2017 Sep 27. PMID: 28718933
Join-Lambert O, Coignard H, Jais JP, Guet-Revillet H, Poirée S, Fraitag S, Jullien V, Ribadeau-Dumas F, Thèze J, Le Guern AS, Behillil S, Leflèche A, Berche P, Consigny PH, Lortholary O, Nassif X, Nassif A. Efficacy of rifampin-moxifloxacin-metronidazole combination therapy in hidradenitis suppurativa. Dermatology. 2011 Feb;222(1):49-58. doi: 10.1159/000321716. Epub 2010 Nov 25. PMID: 21109728.
Rabindranathnambi A, Jeevankumar B. Dapsone in Hidradenitis Suppurativa: A Systematic Review. Dermatol Ther (Heidelb). 2022 Feb;12(2):285-293. doi: 10.1007/s13555-021-00674-x. Epub 2022 Jan 8. PMID: 34997914; PMCID: PMC8850499
Firooz A, Tehranchi-Nia Z, Ahmed AR. Benefits and risks of intralesional corticosteroid injection in the treatment of dermatological diseases. Clin Exp Dermatol. 1995 Sep;20(5):363-70. doi: 10.1111/j.1365-2230.1995.tb01351.x. PMID: 8593711.
García-Martínez FJ, Vilarrasa Rull E, Salgado-Boquete L, Martorell A, Pascual JC, Hernández-Martín Á, Silvente C, Ciudad-Blanco C, Andrés Esteban E, Alfageme-Roldán F. Intralesional corticosteroid injection for the treatment of hidradenitis suppurativa: a multicenter retrospective clinical study. J Dermatolog Treat. 2021 May;32(3):286-290. doi: 10.1080/09546634.2019.1655524. Epub 2019 Aug 29. PMID: 31402725.
Boer J, van Gemert MJ. Long-term results of isotretinoin in the treatment of 68 patients with hidradenitis suppurativa. J Am Acad Dermatol. 1999 Jan;40(1):73-6. doi: 10.1016/s0190-9622(99)70530-x. PMID: 9922015.
Huang CM, Kirchhof MG. A New Perspective on Isotretinoin Treatment of Hidradenitis Suppurativa: A Retrospective Chart Review of Patient Outcomes. Dermatology. 2017;233(2-3):120-125. doi: 10.1159/000477207. Epub 2017 Jun 23. PMID: 28641306.
Patel N, McKenzie SA, Harview CL, Truong AK, Shi VY, Chen L, Grogan TR, Bennett RG, Hsiao JL. Isotretinoin in the treatment of hidradenitis suppurativa: a retrospective study. J Dermatolog Treat. 2021 Jun;32(4):473-475. doi: 10.1080/09546634. 2019. 1670 779. Epub 2019 Sep 26. PMID: 31535587.
Gulliver W, Zouboulis CC, Prens E, Jemec GBE TT. Evidence-based approach to the treatment of hidradenitis suppurativa/acne inversa, based on the European guidelines for hidradenitis suppurativa. Rev Endocr Metab Disord. 2016;17(3):343-351. doi:10.1007/s11154-016-9328-5
Tchero H, Herlin C, Bekara F,Fluieraru S, Teot L. Hidradenitis Suppurativa: A Systematic Review and Meta‑analysis of Therapeutic Interventions. Indian
Journal of Dermatology, Venereology & Leprology. 2019: 85; 248-257.
Zouboulis C, Bechara F, Blok J D, Gulliver W, et al. Hidradenitis
suppurativa/acne inversa: a practical framework for treatment optimization –
systematic review and recommendations from the HS ALLIANCE working group. JEAVD.2019;33:19-31.
Goldburg S, BA Bruce, Strober E, et al. Hidradenitis suppurativa Current and emerging treatments. J Am Acad Dermatol.2020;82:1061-1082.
Patil S, Apurwa A, Nadkarni N. Hidradenitis Suppurativa: Inside and Out. Indian J Dermatol. 2018;63(2):91-98.
Clark AK, Quinonez RL, Saric S, Raja K S. Hormonal therapies for hidradenitis suppurativa: Review. Dermatol Online J. 2017;23(10):6.
Khandalavala BN, Voutsalath Do M. Finasteride in Hidradenitis Suppurativa A “Male” Therapy for a Predominantly “Female” Disease. J Clin Aesthet Dermatol. 2016;9(6):44-50.
A L. Consenso nacional de Hidradenitis supurativa - Guia de tratamiento 2019. Soc Argentina Dermatología. 2019;1(1):1-20.
Vinkel C, Thomsen S. Hidradenitis suppurativa: Causes, features, and current treatments. J Clin Aesthet Dermatol. 2018;11(10):17-23.
Mortimer PS, Dawber RP, Gales MA, Moore RA. A double-blind controlled cross-over trial of cyproterone acetate in females with hidradenitis suppurativa. Br J Dermatol. 1986;115(3):263-268
Sawers RS, Randall VA, Ebling FJ. Control of hidradenitis suppurativa in women using combined antiandrogen (cyproterone acetate) and oestrogen therapy. Br J Dermatol. 1986;115(3):269-274.
Lee A, Fischer G. A case series of 20 women with hidradenitis suppurativa treated with spironolactone. Australas J Dermatol. 2015;56(3):192-196.
Verdolini R, Clayton N, Smith A, Alwash N, Mannello B. Metformin for the treatment of hidradenitis suppurativa: A little help along the way. J Eur Acad Dermatology Venereol. 2012;27(9):1101–1108.
Marasca, C., Annunziata, M. C., Napolitano, M., Fabbrocini, G. (2018). Unconventional therapies for hidradenitis suppurativa. Expert Review of Clinical Pharmacology (9), 879–887. https://doi.org/10.1080/17512433.2018.1509706
Joseph MA, Jayaseelan E, Ganapathi B, Stephen J. Hidradenitis suppurativa treated with finasteride. J Dermatolog Treat. 2005;16(2):75-78.
Alikhan A, Sayed C, Alavi A et al. North American clinical management guidelines for hidradenitis suppurativa: A publication from the United States and Canadian Hidradenitis Suppurativa Foundations: Part I: Diagnosis,
How to Cite
Downloads
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Juan Guillermo Pabón, Ricardo Flaminio Rojas, María Isabel Barona, Beatriz Orozco, Sol Beatriz Jiménez; Esperanza Meléndez; Adriana Motta, Lili Johana Rueda, Claudia González, Viviana Ibagón, Jessica Vallejo, Beatriz Armand, María del Pilar Avellaneda, Edwin Bendek, Carlos Montealegre, Natalia Velásquez, Lina Quiroz, Claudia Uribe, Cristina Lotero, Diego Espinosa, Jaime Rengifo, Rodrigo Nuñez

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |






